| |
| |
| |
Chapter 47: Brain Injury
Clinical Correlation:
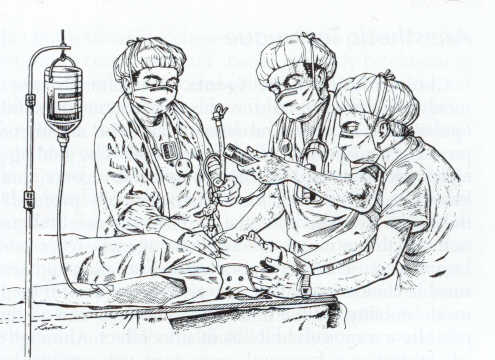
1This case focuses on the management of head injury in begins with the following case description -- a young male (late teens) arrived at the emergency department following a head-on automobile accident.
The patient was both combative and semiconscious upon arrival.
Preliminary neurological assessment indicated that his right arm appeared stronger than his left.
Additionally, a chest contusion was noted consistent with steering wheel impact.
Vital signs: blood pressure 180/100 mm Hg; heart rate 135/min.; hematocrit, 40% and respiratory rate 15/min.
![]()
Some clinical issues:
1-4 (1) An immediate question has to do with the nature of the probable cerebral injury. In this case, without a clear localized neurological syndrome, the probable pathology is cerebral contusion. Cerebral contusion would be associated with swelling (edema) and possibly bleeding. Edema may be secondary to blood brain barrier disruption. CT scans are useful in indentifying cerebral contusion.
In advance of surgical procedures identification of additional neurological injury including cervical spine fracture or basilar fracture is important. Furthermore, contusions can occur below the level of the tentorium [the tentorium is a structure consisting of two dura mater leaves which separates the cerebrum from the brainstem and cerebellum. The brainstem would include the pons and medulla is referred to, along with the cerebellum, as infratentorial. By contrast, the cerebrum is supratentorial.
Brain stem injury may not be initially apparent; however, manifestation postoperatively may be clear in that the patient may not awaken or remains respirator dependent.
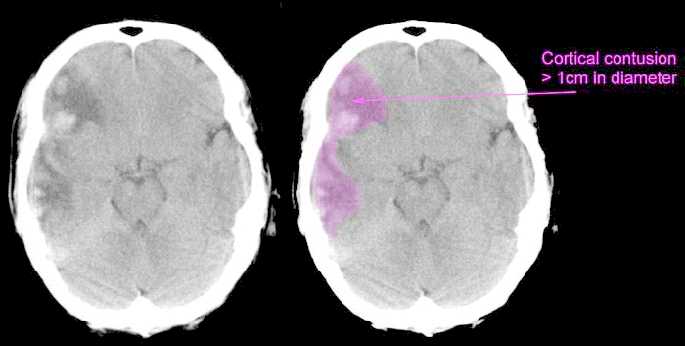 |
"This is a scan of a patient who has sustained a severe head injury. There is extensive bruising of the right side of the brain, showing up as a large, diffuse grey area. You can also see that there are patches of white within the grey area. This represents bleeding. The grey area represents swelling (edema). The area of the cortical contusion is outlined in purple. You will normally find a centimetre scale at the right hand side of a CT scan. This scan would be classified on the Early Outcome Form as "Cortical contusion - greater than 1cm in diameter." Scans provided by Mr Jonathan Wasserberg, Consultant Neurosurgeon; Mr Bill Mitchell, Research Associate, Dept Neurosurgery, University of Birmingham.
(Left) "The image above shows extreme contusion and hemorrhage involving the frontal and temporal poles. These are areas that sit within skull pockets and are commonly injured when the brain moves quickly forward in a severe automobile accident. Note the proximity of the olfactory bulbs to the frontal areas. Patients often lose the sense of smell following these injuries." (Right) "This image illustrates a number of contusions on the brain surface as well as deep within the cerebral convolutions." J. Michael Williams, PhD, Neuropsychology
![]()
|
(2) 1,4,5, 6a,7aInfluence of intracranial hematoma (expanding) on ICP and cerebral perfusion pressure (CPP):
Mass effects of expanding intracranial hematomas results in local and general increases in brain pressure, which causes hemodynamic alterations such as (a) reduced cerebral perfusion pressure and (b) reduced brain blood flow. Neuronal injury is likely to result.
For epidural hematoma CNS pathology often follows from middle meningeal artery tear. Arterial lesions causes rapid and significant neurological deterioration associated with the rapid expansion of the intracranial blood mass within the confines of the cranial vault.
By way of contrast, subdural hematomas, typically following from venous tears, promotes slow evolution of neurological defects often involving patients retaining consciousness after the initial insult and then losing consciousness with neurological deterioration.
6In neuroanesthesia, management of ICP is a critical consideration, both from the point of view of avoiding increases and reducing elevated ICP. A basic concern, assuming a closed cranium, is maintenance of sufficient cerebral perfusion pressure (CPP) to meet neural tissue requirements and in addition present brain tissue herniation between intracranial elements or through the foramen magnum. Cerebral perfusion pressure (CPP) equals mean arterial pressure - intracranial pressure (OR CPP = MAP-ICP) With the cranium open, reduction in ICP creates either improved surgical access or possibly through craniotomy reversal of brain herniation.
 |
 |
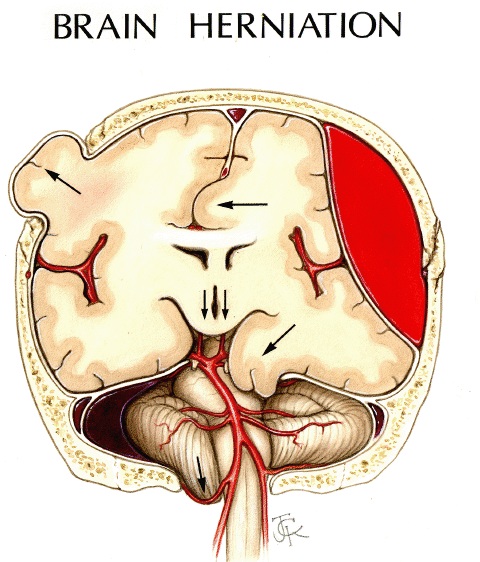 |
Left: 6,7"Schematic representation of various herniation pathways (1) subfalcine, (2) uncal (Transtentorial), (3) cerebellar, and (4) transcalvarium)
Center: Brain herniation refers to displacement of a portion of the brain from its normal position through openings in the inelastic dura secondary to focal or diffuse intracranial pressure. Recognition of the CT signs of brain herniation on the emergent head CT is critical to proper patient management. The types of brain herniations are schematically illustrated...":a) " Subfalcial (cingulate) herniation ; b) uncal herniation ; c) downward (central, transtentorial) herniation ; d) external herniation ; e) tonsillar herniation.Types a, b, & e are usually caused by focal, ipsilateral space occupying lesions, ie., tumor or axial or extra-axial hemorrhage."- Copyright © 2000, 2001 John H. Harris, Jr., M.D. & Thea T. Troetscher, RN, used with permission in accord with site's educational use guidelines.) (Image template: attribution, Gean, AD)
Right: High-resolution image, courtesy of Professor Alisa Gean, MD, University of California, San Francisco, San Francisco General Hospital.13 . Professor Gean has authored the excellent textbook, "Imaging of Head Trauma".
|
|
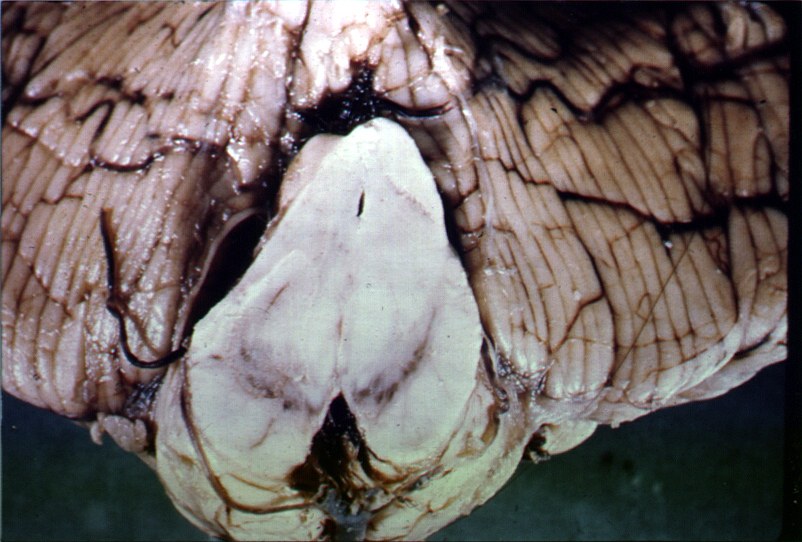 |
(Left)"Bilateral symmetrical infarct of posterior cerebral arteries, secondary to bilateral uncal herniations compressing posterior cerebral arteries" KUMC pathology department, used with permission courtesy of Dr. James Fishback
(Right): "Distortion of midbrain due to uncal herniation. This specimen shows the midbrain in a case in which herniation of medial temporal lobe structures has produced typical distortion of the normal configuration of the midbrain and displacement of midline structures toward the opposite side. Secondary hemorrhages did not develop in this instance " University of Rochester (c), Neuropathology and Neuroimaging Laboratory, Ralph F. Józefowicz, MD John J. Miller, MD James M. Powers, MD
Clinical manifestations of increased ICP: headache (postural, nocturnal awakening patient) nausea & vomiting, somnolence, papilledema, and blurred vision. CT scan findings consistent with ICP elevation include midline shift, loss of sulci, ventricular effacement (if hydrocephalus is present, ventricular enlargement may be observed), edema. On CT scans, edema appear black (hypodense), see below.
|
|
(1) Cystic metastases (2) Perifocal edema Copyright, CID, 17.07.97 ,(C.I.D. (Centre d'Imagerie Diagnostique), Diagnostic Imaging Center, Lausanne, Switzerland)
There are several objectives associated with monitoring the head-injured patient. However, the overall intent is to ensure, if possible, adequate cerebral perfusion/oxygenation while avoiding complications and secondary cerebral injury.
Although we will focus on ICP monitoring a number of other modalities are also important. In the case of intracranial pressure monitoring (ICP) the monitor may be placed in the ventricle, brain tissue (parenchyma), subarachnoid space, subdural space, or epidural space.
Threshold for treatment may be 20-25 mm Hg (LSU limit) with treatment options including surgery if needed, head elevation, mannitol administration, CSF drainage, sedation, paralysis, or barbiturate-induced,. The ICP monitoring as well as other approaches are summarized below:
7Intracranial pressure (ICP) is determined by pressure is associated with blood, brain, and cerebrospinal fluid. Pressure equilibration between these fluids results in a normal ICP of about 0-10 mm Hg. Upper limits of normal range from 15 mm Hg-25 mm Hg, depending on the institution. Also, ICP will be dependent on posture
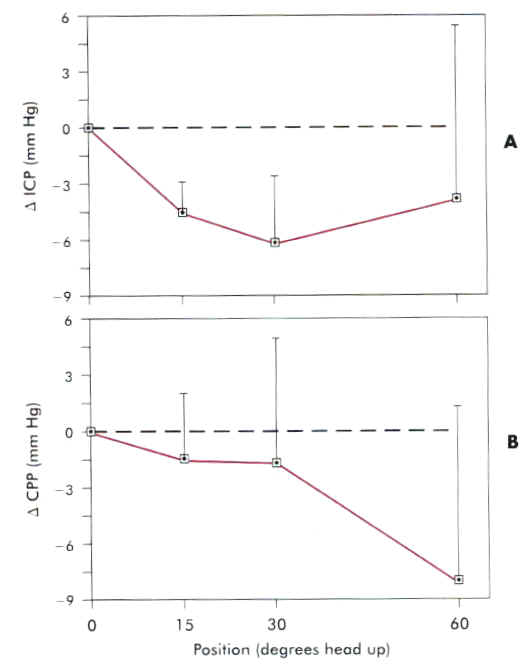 |
As head-up position is increased, ICP may be reduced, but beyond 30o heads-up CPP is likely compromised. Second source: Durward, QJ, Amadner, AL, Del Maestro, RF, et al: Cerebral and vascular responses to changes in head elevation in patients with intracranial hypertension, J Neurosurg 59: 938, 1983.
| Modality | Methodology | Treatment Threshold | Options |
| Intracranial Pressure (ICP) | ICP monitor localized in the ventricle; brain tissue, subarachnoid, epidural or subdural space | 20-25 mmHg (LSU) | Hyperventilation, head elevation, sedation, CSF drainage, paralysis, barbiturate-induced coma or surgery |
| Blood Pressure (CP) | Arterial Line | < 100 mmHg | Vasopressors, fluid, blood replacement |
| Cerebral perfusion pressure (CPP) | CPP=MAP-ICP; MAP = mean arterial pressure | < or equal to 70 mmHg | Control ICP & BP |
| Jugular Bulb venous oxygen saturation SjvO2 | Catheter (often fiberoptic) inserted into the jugular bulb | < 50% saturation | Control ICP & CPP |
| Brain Tissue oxygen monitoring PtiO2 | microcathetic placed into frontal cerebral white matter | < 8.5 mm Hg | Control ICP & CPP |
![]()
|
|
![]()
7ICP monitoring: Indications-
(1) patients with significant head injury (Glasgow Coma Scale 3-8 following resuscitation)
(2) abnormal CT scan revealing contusion, edema, hematoma, compressed basal cisterns.
(3) patient exhibits severe head injury but has a normal CT scan; however, two or more of the following findings are present at admission: age > 40, unilateral or bilateral motor posturing, systolic hypotension (less than or equal to 90 mm Hg. (Reference: Brain Trauma Foundation: Indications for Intracranial Pressure Monitoring, in Guidelines for the Management of Severe Head Injury. Chicago, American Association of Neurological Surgeons, 1995, pp. 5-1-5-25.)
7Approaches for intracranial pressure monitoring: Overview
Catheter tip strain gauge or fiber-optic units are most often used, calibrated before insertion.
Placement: lateral ventricles, parenchyma [using catheter tip pressure transducers], subdural, subarachnoid, or epidural spaces.
7Ranking based on three factors (a) accuracy, (b) stability, and (c) capability of CSF drainage:
1. Intraventricular monitoring device (fluid-coupled or catheter tip pressure transducers);
2. Parenchymal catheter tip transducers;
3. A subdural device again fluid-coupled or catheter tip pressure transducer;
4. The subarachnoid fluid-coupled monitor with external strain gauge (bolt);
5. Epidural monitoring unit.
5Intraventricular catheter: standard method.
The lateral ventricle is penetrated using a nonreactive, soft plastic catheter connected by sterile tubing filled with a saline solution to an external transducer allowing reliable CSF pressure monitoring.
Furthermore, CSF drainage can be accomplished using this catheter. Since reliable pressures depend on ICP transmission through the tubing, any occlusion within the tubing can cause dampened recordings and DOS and correct values.
Difficulties in catheter insertion of being proportional to the extent of brain swelling or the presence of a large mass effect (small ventricles).
Problematic issues with this approach also include catheter-induced hematoma, tissue injury, and infection, although infection seems to be less likely within the first 4 days following placement. Accordingly, prolonged monitoring (i.e. > 4 days) would require placement of the catheter at a different side.
5As noted in the figure above also, the subdural-subarachnoid bolt involves a hollow screw anchored to the calvarium with the tip passing through the dura (incised).
A clear advantage is that knowledge of ventricular position is unnecessary and there is minimal risk of brain tissue injury.
Reasonable placement obviates the possibility of damaging a major venous sinus.
On the other hand, the bolt method cannot be used to provide CSF drainage thereby lowering ICP or to evaluate brain tissue compliance.
Since the bolt is connected to the pressure transducer with tubing again filled with sterile saline, incorrect measurements would occur with tubing blockage.
In addition to this problem, brain structure can obstruct the tip thus preventing accurate recordings. A way around this problem involves drilling side holes near the tip, thus reducing the impact of possible tip blockade.
5Subdural ICP monitoring devices have the advantage of easy placement; however, they may become loose or malfunction if coplanarity to the brain surface is lost.
Infection is a particular problem with subdural monitoring -- the infection may be localized or may manifest as meningitis or osteomyelitis.
5Epidural transducers are usually of one of two varieties: (1) this device has a pressure-sensitive membrane located either close to or in direct contact with the dura whereas the second device (2) called a Ladd epidural transducer utilizes the Numoto pressure switch approach, which involves a pressure-indicating bag implanted into epidural space and connected using an enclosed fluid column to an extracranial sensor.[Numoto M, Slater J, Donaghy MP (1973) An implantable switch for monitoring intracranial pressure. J Neurosurg 39 (1973): 784-787 ]; Extradural placement reduces infection risk, although there are some disadvantages. Disadvantages include placement difficulty and bleeding risk. Epidural transducers obviously cannot be used to provide CSF drainage or to assess intracranial compliance.
5Miniaturized Fiberoptic Devices
Miniaturized fiber-optic monitoring devices are relatively new with the sensing element mounted at the distal part of a 4-French fiber-optic bundle. This device is inserted through a 2-mm burr hole.
The sensing device records changes in light reflectance of a pressure-sensitive diaphragm at the fiber-optic catheter tip. A mean pressure can be displayed numerically or in terms of a pressure waveform.
The tip may be placed in the subdural, intraventricular, or intraparenchymal volumes. The solid-state physical construction eliminates leaks, catheter occlusion and reduces "drift" associated with fluid-or air-filled systems. Infection risk is also attenuated. Drift with the system may be a problem after five days, since recalibration is not an option in situ.
The most current fiber-optic ICP monitoring systems support assessment of many parameters including ICP, local cerebral blood flow (CBF) by means of laser Doppler flowmetry, brain tissue oxygen pressure (PO2), carbon dioxide pressure (PCO2), and pH. By analyzing ICP, local CBF, and brain tissue oxygenation data, ischemia may be identified earlier and an interventional therapeutic efficacy more readily determined.
7Intracranial Pressure Waves:
"B" waves reflect slow respiratory fluctuations in ICP--exhibiting intervals of 30 secs to 2 minutes and ranging in amplitude from about 10-50 mm Hg
"C" waves represent the smaller cardiac fluctuations in ICP.
"A" waves are not shown above, but represent long lasting waves (several minutes) indicative of diffuse cerebral ischemia, and often precede herniation. "A" waves therefore represent an interaction of cerebrovascular regulation in the context of significantly diminished intracranial compliance
 |
"These 'A'-waves (plateau waves) result when mean systemic blood pressure decreases below threshold (and thus cerebral perfusion pressure) CPP falls below the ischemic threshold. Cerebrovasodilation then occurs in response. In a non-compliant cranium, this vasodilation results in greatly increased intracranial pressure." picuBOOK an on-line resource for pediatric critical care, Joseph V. DiCarlo MD, Division of Pediatric Critical Care Medicine, Lucile Packard Children's Hospital, Stanford University, Palo Alto California 94304 USA
![]()
 |
 |
 |
(Left) Image courtesy of Grant's Atlas of Anatomy http://www.veins1.com/reference/PreviewCategory.cfm/1/9; (Center, Right) Images from 9Using Jugular Venous Catheters in Patients with Traumatic Brain Injury, Kidd, KC and Criddle, L, Critical Care Nurse, vol. 21, No. 6, December 2001 original reference: http://www.aacn.org/pdfLibra.NSF/Files/Casey/$file/Casey.pdf
9The internal jugular vein drains cerebral blood in a manner that results in limited contamination from extracerebral sources. Cerebral oxygen consumption is observed as a difference between arterial oxygen saturation and jugular bulb oxygen saturation (SaO2 - SjvO2). Brain oxygen consumption is tightly regulated; however, in the presence of brain injury, this autoregulation process operates abnormally causing mismatching between cerebral blood flow (CBF) and cerebral metabolic requirements. SjvO2 monitoring provides insight into factors influencing tissue oxygenation and oxygen consumption.
5, 9For example, cerebral oxygen desaturation reflected in the jugular bulb readings may occur within two days following traumatic brain injury. With normal SaO2 and PaCO2, SjvO2 should range between 60% and 80%; moreover hypoxemia is suggested if SjvO2 falls to less than 55%. Hyperemia (oxygen supply exceeding metabolic requirement) is suggested by SjvO2 values >75%. Elevation of SjvO2 may suggest neuronal death since this condition results in diminished oxygen consumption.
5Hyperemic states could follow from reduced metabolic need (coma, brain death) or from excessive CBF (e.g. severe hypercapnia. The hypoxemia indicated by SjvO2 falling to less than 55% could herald ischemic brain damage. SjvO2 of less than 55% may be caused by increased metabolic requirement such as that accompanying seizures or fever providing such increased requirement is not matched by an commensurate enhancement of flow. Alternatively, SjvO2 falling to less than 55% can also just reflect inadequate flow. Finally, systemic blood oxygenation state would influence in a more fundamental way jugular bulb saturation.
5Despite the limitation of not detecting focal ischemia, jugular bulb venous oximetry can assist diagnosis of cerebral ischemia, excessive hyperventilation, or inadequate perfusion pressures.
Sensors available for brain tissue assessment combine determinations of PO2, PCO2, pH and temperature. The electrode is associated with a fiber-optic system; the system was originally developed for continuous intra-arterial blood gas monitoring and consists of a sterile and disposable unit that includes two optical fibers for PCO2 and pH measurement, and a small "Clark" PO2 measurement electrode and a thermocouple for temperature assessment. A dialysis catheter, furthermore allows measurement of metabolic markers such as glucose, excitotoxic amino acids (e.g. amino acids which act as neurotransmitters or neuromodulators that cause EPSPs), and lactate. This type of sensor is clearly invasive since it requires placement into cortical tissue and measurement so obtained are limited to the tissue which is being directly assessed and may not necessarily reflect global oxygenation/metabolic activities.
"The oxygen electrode is a simple device in which a current proportional to [O2] is generated by polarization of a Pt-electrode to reduce the O2. The configuration used for measuring respiration or photosynthesis is that suggested by Clark (the Clark oxygen electrode), and available in many commercial forms. In this configuration, the Pt-electrode area is kept small, so as to minimize the rate of consumption of oxygen, and the Pt and reference electrodes are separated from the reaction medium by an oxygen permeable membrane."--(A. R. Crofts), University of Illinois at Urbana-Champaign, Biophysics 354;
"These electrodes have a thin organic membrane covering a layer of electrolyte and two metallic electrodes. Oxygen diffuses through the membrane and is electrochemically reduced at the cathode. There is a carefully fixed voltage between the cathode and an anode so that only oxygen is reduced. The greater the oxygen partial pressure, the more oxygen diffuses through the membrane in a given time. This results in a current that is proportional to the oxygen in the sample. Temperature sensors built into the probe on some advanced measurement systems allow compensation for the membrane and sample temperatures, which affect diffusion speed and solubility. The meter uses cathode current, sample temperature, membrane temperature, barometric pressure and salinity information to calculate the dissolved oxygen content of the sample in either concentration (ppm) or percent saturation t% Sat). The voltage for the reduction can either be supplied electronically by the meter (potentiometric oxygen electrode) or dissimilar metals may be used for the two electrodes, picked so that the correct voltage is generated between them (galvanic electrode).
"Clark had the ingenious idea of placing very close to the surface of the platinum electrode (by trapping it physically against the electrode with a piece of dialysis membrane) an enzyme that reacted with oxygen. He reasoned that he could follow the activity of the enzyme by following the changes in the oxygen concentration around it, thus a chemosensor became a biosensor. Based on this experience and addressing his desire to expand the range of analytes that could be measured in the body, he made a landmark address in 1962 at a New York Academy of Sciences symposium in which he described how "to make electrochemical sensors (pH, polarographic, potentiometric or conductometric) more intelligent" by adding "enzyme transducers as membrane enclosed sandwiches". The concept was illustrated by an experiment in which glucose oxidase was entrapped at a Clark oxygen electrode using dialysis membrane. The decrease in measured oxygen concentration was proportional to glucose concentration. In the published paper (Clark, L.C. Jnr. Ann. NY Acad. Sci. 102, 29-45, 1962), Clark and Lyons coined the term enzyme electrode. Clark's ideas became commercial reality in 1975 with the successful re-launch (first launch 1973) of the Yellow Springs Instrument Company (Ohio) glucose analyser based on the amperometric detection of hydrogen peroxide. This was the first of many biosensor-based laboratory analysers to be built by companies around the world."--This text has been compiled from the biography of Clark available in the Internet.
![]()
1,8a (3)What are the consequences of arterial hypertension in head injury patients?
Following acute head trauma there is a tendency for reduced cerebral blood flow, even though normal mean arterial pressures are present.. Hypertension, possibly due to catecholamine release, may also be observed and one interpretation is that cerebral perfusion may benefit when a high arterial pressures which opposes trauma-induced elevated intracranial pressures. In the absence of the intact autoregulatory system, a somewhat elevated mean arterial pressure may be beneficial. Certainly the hypotensive condition should be avoided since in the presence those increased intracranial pressure, hypotension promotes neuronal damage.
5Serious intracranial hypertension can cause a reflex arterial hypertension with bradycardia, also known as Cushing's triad. Reduction in systemic pressure can worsen cerebral edema by decreasing cerebral perfusion pressure (CPP). In this clinical situation, systemic blood pressure may be lowered slowly (in the presence of high intracranial pressures) and doing so may disrupt the reflex response.
|
|
8In the absence of the normal autoregulatory cerebrovascular perfusion system (-- line) abnormally low cerebral blood flow can occur even with relatively normal mean arterial pressures. In the presence of head injury or subarachnoid hemorrhage, then, inadequate cerebral perfusion can occur even with reasonable, normotensive blood pressures. Even slight hypotensive responses are sufficient to promote cerebral ischemia.[Bouma GJ, Muizelaar JP, Choi SC et al: Cerebral circulation and metabolism after severe traumatic brain injury: The elusive role of ischemia. J Neurosurg 75: 685, 1991; Ishii, R: Regional cerebral blood flow in patients with ruptured intracranial aneurysms. J Neurosurg 50: 587, 1979.]
![]()
1 (4) The role of mannitol administration in this patient
With intracranial mass lesions (e.g. hematoma, tumor) mannitol will induced a rapid ICP decrease without rebound. Historically, there was concerned that if the head injury induced a blood brain barrier disruption, then mannitol by diffusing into the brain might actually increase ICP. This concerned has been outweighed by the benefits those mannitol and mannitol is a cornerstone of many head injury protocols.The principal mannitol mechanism of action is that of osmotic diuresis in which the presence of intravascular mannitol induces a net fluid flux from the brain into the blood.
10Mannitol: "Mannitol (Osmitrol, Resectisol) -- May reduce subarachnoid space pressure by creating osmotic gradient between CSF in arachnoid space and plasma. Not for long-term use. Initially assess for adequate renal function in adults by administering test dose of 200 mg/kg, given IV over 3-5 min; should produce urine flow of at least 30-50 mL/h of urine over 2-3 h. Same test in children should produce urine flow of at least 1 mL/kg/h over 1-3 h."
10Adult Dosage: "1.5-2 g/kg IV as 20% solution (7.5-10 mL/kg) or as 15% solution (10-13 mL/kg) over period as short as 30 min"
10Pediatric Dosage: "Initial dose: 0.5-1 g/kg IV Maintenance dose: 0.25-0.5 g/kg IV q4-6h"
10Contraindications: "Documented hypersensitivity; anuria; severe pulmonary congestion; progressive renal damage; severe dehydration; active intracranial bleeding; progressive heart failure"
10Pregnancy: "C - Safety for use during pregnancy has not been established. "
10Precautions: "Carefully evaluate cardiovascular status before rapid administration since sudden increase in extracellular fluid may lead to fulminating CHF; avoid pseudoagglutination; when blood given simultaneously, add at least 20 mEq sodium chloride to each liter of mannitol solution; do not give electrolyte-free mannitol solutions with blood"
5Mannitol as part of Management of Intracranial Hypertension (severe head injury)
Initiate ICP monitoring
Insure CPP . 70 mmHg
Respond to intracranial hypertension using First Tier therapy approaches
Ventricular drainage if possible
Mannitol (0.25 - 1 g/kg iv); may be repeated if serum osmolarity <320 mOsm/L and if the patient is euvolemic
Hyperventilation to PaCO2: of 30-35 mm Hg
Respond to intracranial hypertension using Second Tier therapy if needed
Hyperventilations to PaCo2 < 30 mmHg (monitoring of the following parameters recommended: (a) jugular bulb oxyhemoglobin saturation (b) areteriovenous difference in oxygen content and /or (c) cerebral blood flow
High-dose barbiturate administration
Possible implementation: hypothermia
Possible implementation: hypertensive treatment
Possible implementation: Decompressive craniectomy
![]()
1 (5) Intubation issues: Risks and benefits associated with endotracheal intubation in the emergency room setting
Intubation in principle protects against aspiration/regurgitation of stomach contents if airway reflexes are compromised secondary to injury. Also,CO2 retention as a result of diminished ventilatory drive and/or soft-tissue obstruction of the upper airway may occur. In the former case, aspiration pneumonitis is a significant complication and can cause prolonged ICU stay. Increased CO2 retention can lead to increase cerebral blood flow & blood volume, factors which resulted ICP elevation. Both of the above factors can result in hypoxemia, a contributing factor to the frequency of mortality and and injury patients.
If the patient is combative, intubation may be problematic. Endotracheal intubation in this context can precipitate elevations in blood pressure and other cardiovascular responses that worsen the developing intracranial injury. Cervical spine x-ray is required to document normal C1-C7 anatomy prior to intubation in order to avoid exacerbating spinal injury. In this case, a semiconscious patient may not be cooperative during x-ray. If endotracheal intubation were required, the intubation approach in the emergency department setting would be comparable to that in the operating room.
The following sequence would apply:
preoxygenation
defaciculation using a nondepolarizing muscle relaxant
cricoid pressure for esophageal occlusion
brief general anesthesia induced using IV thiopental (3-4 mg/kg) and lidocaine (1.5 mg/kg) and muscle relaxation by succinylcholine (Anectine) (1.5 mg/kg).
Following attainment of the secure airway, hyperventilation to a PaCO2 of about 30 mm Hg may be initiated
11Assessment of cervical spine:
Prior to intubation the status of the cervical spine in the trauma patient must be assessed. Relatively low-risk criteria have been enumerated that may be used to exclude cervical spine fractures. These criteria focus on both patient history and physical examination. The criteria for ruling out cervical spine fractures using clinical assessment include:
(1) "patient is not complain of neck pain when asked" AND
(2) "patient does not have neck tenderness on palpation" AND
(3) "patient does not have any history of loss of consciousness" AND
(4) "patient does not have any mental status changes resulting from trauma, alcohol, drugs, etc." AND
(5) "patient has no symptoms referable to a neck injury, such as paralysis, sensory changes (including transitory symptoms now result), etc." AND
(6) "patient has no other distracting painful injury such as fractured ankle, fractured ribs, etc."
11A radiographic evaluation of the patient should include a true lateral view, which allows visualization of all seven cervical vertebrae as well as the C7-T11 junction, an anteroposterior and an open-mouth odontoid. An adequate cerebral spine visualization may require the patient to extend one arm above the head (assuming no arm injury).
Therefore, any radiological evaluation the does not include the three views noted above as well as the C7-T1 junction would not be adequate. The patient should remain in cervical immobilization and plain films repeated or CT scans obtained until all vertebrae can be readily assessed. The most frequent reason all of overlooked spinal injury tends to be an adequate film series as opposed to film misinterpretations. Furthermore, in addition to the three views noted above, some suggest adding to lateral oblique views routinely. Other attitudes concerning lateral oblique imaging depend on the need to resolve a question of fracture suggested on the other three films for if the other films do not adequately visualized the cervicothoracic junction.
|
|
11Schematic lateral view of the cervical spine. Note the odontoid (dens), the predental space and the spinal canal. (A=anterior spinal line; B=posterior spinal line; C=spinolaminar line; D=clivus base line) (c) 1999 David Klemm;
11"A type II dens fracture. Lateral radiograph shows a fracture through the base of the odontoid process (dens) with the dens and C1 posterior to C2 (arrow indicates fractured base of dens)." Figure on right (c) 1999 David Klemm;
12"Fractures of the dens are commonly classified according to a scheme proposed by Anderson and D'Alonzo into types I, II, and III. Type II fractures are the most common, and consist of a fracture through the base of the dens, at its junction with the C2 body. Type II fractures have a very high incidence of nonunion if not surgically fused. If the fracture extends through the upper body of C2, it is classified as type III. Type III fractures usually heal completely with external immobilization. The type I fracture is an avulsion fracture of the tip of the dens. This is an extremely rare injury."
11"Jefferson fracture. Anteroposterior tomogram at the craniocervical junction demonstrates lateral mass of C1 (arrows) lying lateral to the lateral masses of C2 (arrowheads) on both the left and right sides as a result of spread of the ring of C1. Figure on right (c) 1999 David Klemm; "
 |
 |
11"Jefferson fracture. Computed tomographic image through ring of C1 shows the anterior arch fracture (small arrow). Another small fragment (curved arrow) is shown lateral to the dens. The posterior arch fracture (arrowhead) on the right is not clearly demonstrated on this cut. Figure on right (c) 1999 David Klemm; "
11"Hangman's fracture. Lateral radiograph reveals markedly increased prevertebral swelling (two short arrows) associated with the fracture at the posterior aspect of C2 pedicles (medium arrow). Displacement is obvious by following the posterior spinal line (long arrow).Figure on right (c) 1999 David Klemm;"
| Spine Level | Fracture | Stability Assessment | Mechanism/Clinical Comment | Radiological Assessment |
|
C1 |
Jefferson Fracture | Moderately Stable | Burst Fracture; follows from axial load or vertebral compression | Displaced lateral aspects of C1 on odontoid view, predental space > 3 mm |
|
C1 |
Alantoaxial subluxation | Highly Unstable | Occurs in Down's syndrome patients, rheumatoid arthritis and similar disease | Asymmetric lateral bodies on odontoid view, increased predental space |
|
C2 |
Odontoid fracture | Highly unstable | unclear | may require CT for adequate visualization |
|
C2 |
Hangman's fracture | Unstable | occurs with sudden deceleration (hanging) and with hyperextension as in automobile accidents | "Bilateral pedicle fracture of C2 with or without anterior subluxation; lateral view is required" |
|
Any Level |
Flexion teardrop injury | Highly unstable | Sudden and forceful flexion | "Large wedge off the anterior aspect of affected vertebra; ligamentous instability causes alighment abnormalities" |
|
Any Level |
Bilateral facet dislocations | Highly unstable | Flexion or combined flexion/rotation | "Anterior displacement of 50% or more of one cervical vertebra on lateral views" |
|
Any Level |
Unilateral facet dislocations | Unstable | Flexion or combined flexion/rotation | "Anterior dislocation of 25 to 33% of one cervical vertebra on lateral views; an abrupt transition in rotation so that lateral view of affect vertebra is rotated; lateral displacement of spinous process on anteroposterior view" |
|
Lower or cervical or upper thoracic |
Clay shoveler's fracture | Very stable | Flexion, such as when picking up and throwing heavy loads (such as snow or clay) | "Avulsion of posterior aspect of spinous process; frequently an incidental finding" |
5In head injury there is a significant incidence of cervical spine damage in surviving patients.
For adults the incidence is about 1%-3% in about 0.5% for children.
When one considers motor vehicle accidents which occur at high speed or those individuals who experience head-first falls, cervical spine injury is more common, greater than 10% of actual cervical spinal fracture.
5Cross-table lateral radiographic view may miss 20% of these fractures. As noted earlier, additional views are required and when these techniques are implemented about 93% of fractures are diagnosed. If cervical spine fracture cannot be excluded by radiographic assessment and emergent intubation is required, in-line stabilization is appropriate. Note that axial traction is not recommended due to spinal cord distraction injury risk.
 |
5, 6,6bFollowing a hypnotic and muscle relaxant administration intubation proceeds even if the cervical spinal status is uncertain. In this method, one assistant maintains in-line stabilization with the occiput held firmly to the backboard (hands are placed along the side of the head with fingertips on the mastoid holding the occiput down) . The second assistant applies cricoid pressure. Note that the posterior portion of the cervical collar remains in place.
6The approach involving oral intubation with anesthesia and relaxation with in-line stabilization with the patient's occiput held securely on the backboard has been determined to be reasonable based on clinical trials. However, this orientation limits attainment of the "sniff" position and makes laryngoscopy more challenging.
The point however is to reduce atlanto-occipital (A-O) motion. Normal laryngoscopy is associated with significant A-O extension, an important point given that devastating spinal cord injury may be often associated with atlanto-occipital region pathologies which happened to be difficult to assess radiologically.
With the patient secured on the backboard has described earlier, visualization of the glottis may proceed with a relatively reduced degree of A-O extension. Laryngoscopy in this situation reduces A-O extension probably because of greater compression of the soft tissue structures of the tongue and mouth floor (compression involves performing laryngoscopy against the assistant's counterpressure).
For a number of reasons including radiologic evidence of instability, significant pre-existing neurological deficit, or if neck movement is associated with severe pain, alternative intubation approach is can be considered.
8Awake fiber-optic intubation and then awake positioning, as noted earlier, is one approach. Moreover, newer airway management instruments such as the Bullard laryngoscope, light wand, or Augustine intubating airway may be considered.
 |
 |
 |
5Should facial fractures with soft tissue edema make larynx visualization impossible or difficult, fiber-optic intubation or intubation using an illuminated stylet may be tried.
As we will consider shortly, in the presence of a suspected basal skull fracture or severe facial fractures, nasal intubations are avoided.
In the absence of facial injury, the most appropriate approach would be rapid-sequence induction using cricoid pressure while maintaining in-line stabilization.
5Note that all head-injured patients are assumed to have full stomach.
If the patient is severely injured, awake, oral intubation without anesthetic agents might be possible; however, this approach is less likely in the awake, combative/uncooperative individual.
As a general rule, essentially any intravenous induction drug (except ketamine) might be used, although the choice of muscle relaxants may be somewhat less clear since succinylcholine can increase intracranial pressure (ICP).
Transient increases in ICP due to succinylcholine may be less important than a pharmacokinetic properties of succinylcholine (rapid onset/elimination) given that the patient may have acute airway problems, full stomach, and also there is a clinical need to perform subsequent neurological assessments.
As noted earlier also, control of the airway as a first step is then followed by cardiovascular resuscitation with an interest in avoiding the common occurrence of transient hypotension and furthermore the avoidance of more prolonged hypotension due to systemic injury causing hemorrhage. The hypotensive state contributes to a significant reduction in cerebral perfusion pressure which predisposes to extensive neurological injury.
![]()
1 (6) Question about the use of succinylcholine as part of the regiment for endotracheal intubation: risks vs. benefits
Succinylcholine is responsible for a slight increase intracranial pressure (ICP).
However, this increase is transient and can be blocked if need be by preceding dose of metocurine (0.03 mg/kg. Other curariform nondepolarizing muscle relaxant agents (defasciculating dose) would also expected to block succinylcholine-induced transient ICP elevation.
The central point is that for emergent rapid induction sequencing, the risks associated with succinylcholine use in a patient with possibly acute airway compromise, full stomach, and the need to provide prompt neurological assessments are small compared to the risks of not using succinylcholine to avoid a transient ICP increase.
![]()
1(7) Should nasal intubation the use in the patient who is blood visible behind one eardrum?
1,6,9a The "Battle" sign or other evidence slowing basal skull fracture (e.g. CSF rhinorrhea) usually contraindicates nasal intubation. However, the nasal route can be used despite concerns about entering the cranial vault via a skull base fracture; but, discretion must be used and special sensitivity to unusual resistance encountered in endotracheal tube passage exhibited. The nasal route should definitely be avoided in the presence of obvious facial crush injury. At all events, a nasally-placed endotracheal tube will ultimately require replacement due to patency difficulty for because of maxillary sinusitis risk.
 |
"Battle's sign is bruising over the mastoid sinus (just behind the auricle) and is a delayed physical finding associated with basilar skull fractures. Hemotympanum (blood behind the ear drum) and "raccoon eyes" (periorbital bruising) are other delayed findings consistent with basilar skull fractures." San Francisco General Hospital Emergency Services, Clinical Images
 |
"A 15 year old male presents to the Pediatric ER one day after being released from the hospital. He had been admitted for observation for 24 hours status post falling off the hood of a car travelling 10 MPH. He had had loss of consciousness for 10 minutes. CT scan of the head and neck were negative during the hospitalization. Since discharge, he had progressively worsening headache and vomiting. Bleeding from the left ear, which began during the hospitalization, had continued. His vital signs were normal, and his neurologic exam was only notable for his desire to sleep. His left ear is pictured (above)." ['Battle's sign' - A high resolution CT scan with thin axial and coronal cuts demonstrated a temporal bone or 'basilar' skull fracture. The patient had also developed a large parietal epidural hemorrhage with shift of structures that required emergent drainage. Remember this case the next time you are thinking that the negative predictive value of an early head CT s/p trauma is 100%.]--© Jay D. Fisher MD 10/31/00
![]()
1,10a,11a(8) What is the importance of computed tomography (CT scanning) in early evaluation of head injury patients?
CT scanning is the diagnostic test of choice to determine magnitude of head injury and the possible requirement for emergent surgery.
Following contrast injection, tomographic images can provide information about the presence of large intracranial hematomas sufficient to induce mass effect shifts which would require surgical intervention without delay.
By contrast, the absence of mass effect accompanied by lack of evidence of lateral ventricular compression or compression of basal cisterns could predispose to more conservative management.
Nonetheless, decompressing craniectomy might be performed in the unconscious patient based on the ICP monitoring, when ICP values exceed 20-30 mm Hg despite efforts to control pressure using pharmacological intervention (mannitol and barbiturate anesthesia) and hyperventilation toPaCO2 = 20-25 mm Hg.
![]()
1(9) Is there a value for chest x-rays in this patient?
Intraoperative catastrophic ocurrences include so-called intra-abdominal bleeding.
Other catastrophes include cervical spine injury and unexpected intrathoracic derangements.
In motor vehicle accidents, steering wheel, may induce cardiac or pulmonary contusion, great vessel laceration or hemopneumothorax. Consequently, excluding these possibilities by CT scanning is important. Furthermore, some assessment concerning these issues prior to CT scanning can be made.
For example, pulmonary contusion, if suspected can be managed with a chest tube prior to tension pneumothorax development-particularly important if the patient will be receiving positive pressure ventilation. A widened mediastinum or other indications of great vessel injury may require operative management of the major vascular injury taking precedence over the head injury.
![]()
1(10) Suppose the electrocardiogram indicates inverted T-waves in the precordial leads. What are possible causes and would be these T-waves necessarily indicate myocardial injury? Will be the consequence of pericardial blood with respect to the ECG?
Neuropathology may be associated with inverted T-waves, particularly ruptured intracranial aneurysms.
Ventricular bleeding or bleeding into the basal cisterns also induce electrocardiographic changes.
In this setting, therefore, such changes may not indicate myocardial ischemia/injury.
In the event of cardiac contusion (steering wheel trauma) ventricular arrhythmias may develop and ST segmental elevation in the precordial leads are often exhibited. Pericardial cavity blood may be inferred if the ECG shows low voltage and heart sounds are muffled.
![]()
1Bedford, R.F., "Head Injury" in Anesthesiology: Problem-Oriented Patient Management (Fun-Sun F. Yao, editor),4th edition, Lippinottt Williams & Wilkins, Philadelphia, pp 492-503, 1998 (secondary cited sources below)
2Cohen, W: Imaging and determination of posttraumatic spinal instability. In: Cooper PR (ed): Management of Post-Traumatic Spinal Instabilty: Neurosurgical Topics, Vol 2, p 19. Park Ridge, IL, AANS Publications, 1990.
3Eisenberg HM, Gary HE Jr, Aldrich EF et al: Initial CT findings in 753 patients with severe head injury, J Neurosurg 73: 688, 1990.
4Lotato RD, Sarabia R, Cordobes F et al: Post-traumatic cerebral hemispheric swelling. J Neurosurg 49: 530, 1988.
5aEisenberg, HM, Gary HE Jr, Aldrich EF et al: Initial CT findings in 753 patients with severe head injury J. Neurosurg 73: 688, 1990
6aSeelig, JM, Becker DP, Miller, JD et al: Traumatic acute subdural hematoma: Major motality reduction in comatose patients treated within four hours. N Engl J Med 304: 1511, 1981
7aYoshino E, Yamaki T, Higuchi, T et al: Acute brain edema in fatal head injury: Analysis by dynamic CT scanning J. Neurosurg 63: 830, 1985.
8aNagai H, Kamiya K, Ishii S (eds): Intracranial Pressure IX, pp 222-224. Tokyo, Springer-Verlag, 1994
9aGrindlinger GA, Neihoff, J, Hughes, L et al: Acute paranasal sinusitisk related to nasotracheal intubation of head-injured patients. Crit Care Med 15:214 1987.
10aCruz, J An additional therapeutic effect of adequate hyperventilation in severe acute brain trauma: Normalization of cerebral glucose uptake. J Neurosurg 82: 379, 1995
11aSaul TG, Ducker, TB: Effect of intracranial pressure monitoring and aggressive treatment on mortality in severe head injury. J Neurosurg 56: 498, 1982.
5Bendo, AA, Kass, IS, Hartung, J and Cottrell, JE "Anesthesia for Neurosurgery, Chapter 28, in: Clinical Anesthesia, 4th ed, Barash, PG, Cullen, BF, Stoelting, RK (eds) pp 777-789, Philadelphia, PA., Lippincott Williams & Wilkins, 2001
6Drummond, JC and Patel PM "Neurosurgical Anesthesia, Chapter 52, In Anesthesia (Ronald D. Miller, ed), 5th edition, Churchill-Livingstone, Philadelphia, pp 1895-1933.
Fishman, RA: Brain edema. N Engl J Med 293: 706, 1975
6bStene JD: Anesthesia for the critically ill trauma patient. In Siegel JH (ed): Trauma: Emergency Surgery and Critical Care. New York, Churchill Livingstone, 1987.
7Awasthi, D. Multimodal Monitoring in Patients with Head Injury, Louisiana State Medical Center, http://www.medschool.lsumc.edu/Nsurgery/monitorheadinj.html
8Todd, MM, Warner, DS and Maktabi, MA, "Neuroanesthesia: A Critical Review", Chapter 67, In Principles and Practice of Anesthesiology 2nd edition, Longnecker, DE, Tinker, JH, and Morgan Jr, GE,eds, pp 1607-1658.
9Kidd, KC and Criddle, L, Using Jugular Venous Catheters in Patients with Traumatic Brain Injury, Critical Care Nurse, vol. 21, No. 6, December 2001
10Olson, DA, Consulting Staff, Department of Neurology, Atlanta Medical Center, "Head Injury: eMedicine, May 2001, http://www.emedicine.com/NEURO/topic153.htm
Editor(s): Joseph Carcione, Jr, DO, Assistant Professor, Department of Neurology, Albert Einstein College of Medicine;
Francisco Talavera, PharmD, PhD, Senior Pharmacy Editor, eMedicine; Florian P Thomas, MD, PhD, Drmed, Associate Program Director, Associate Professor, Departments of Neurology, Molecular Virology, Molecular Microbiology, and Immunology, Saint Louis University School of Medicine; Matthew J Baker, MD, Consulting Staff, Collier Neurologic
Specialists, Naples Community Hospital; and Nicholas Lorenzo, MD, eMedicine Chief Publishing Officer, Chief Editor, eMedicine Neurology; Consulting Staff, Neurology Specialists and Consultants
11Graber MA and Kathol, M "Cervical Spine Radiographs in the Trauma Patient "American Family Physician, January 15, 1999, (c) American Academy of Family Physicians http://www.aafp.org/afp/990115ap/331.html
12Smith, JK .University of North Carolina Department of Radiology UNC Radiology Teaching File, Musculoskeletal Section, Case #6 http://www.ibiblio.org/jksmith/UNC-Radiology-Webserver/Bone/B6.html
13Gean AD Imaging of Head Trauma, Lippincott Williams & Wilkins, 1994.