-
Overview amebiasis
-
Causative agent of amebiasis: protozoan parasite Entamoeba
histolytica
-
Diagnostic Criteria:
-
Suggestive:
-
Definitive:
-
Cysts or
trophozoites in stool or
rectal biopsy or
trophozoites in other
organs, e.g. the liver
-
95%
sensitivity of serology
in patients with
extraintestinal amebiasis
-
Clinical
Manifestations-Subjective
-
Clinical Manifestations:
Objective
-
Intestinal
Amebiasis
-
Extraintestinal
Amebiasis (amebic liver abscess)
-
Physical
Exam:
-
Most Important
Sign: Liver enlargement +
pain on palpation (point
tenderness, a frequent
finding)
-
If
abscess located high
under diaphragm:
-
Laboratory:
-
Differential Diagnosis
(Primary
Reference: Morgan, Juliette and
del Rio, Carlos, Amebiasis in Medicine for the Practicing
Physician (Hurst, J. W., ed) Appleton-Lange, 1996, pp.
457-459.)
-
Overview:-intestinal amebiasis
-
Intestinal Amebiasis:
-
Diagnostic
key: stool examination {routine lab
tests: not useful}
-
Difficulties in
performing correct stool examinations
-
Common
false-positives and
false-negatives
-
Should
take multiple stool samples (one
"negative" stool result
is not sufficient to rule out
intestinal amebiasis)
-
Samples must be
properly maintained if not
analyzed immediately
-
Presence of many
fecal leukocytes suggests some other
diagnosis since E. histolytica
causes lysis of neutrophils
-
Indirect hemagglutination
test: 70% sensitivity in patients with
active intestinal disease-- only 10%
sensitivity in asymptomatic cyst carrier
-
Overview: Extraintestinal Amebiasis:-
-
Differential includes:
-
Pyrogenic abscess
-
Metastatic/primary
tumor (includes hemangioma)
-
Typical amebic abscess:
-
Extraintestinal Amebiasis:
-
Summary
of Clinical Features:
-
"A
wide spectrum, from
asymptomatic carriers
("luminal
amebiasis"), to
invasive intestinal
amebiasis (dysentery,
colitis, appendicitis,
toxic megacolon, amebomas), to invasive
extraintestinal amebiasis
(liver abcess,
peritonitis,
pleuropulmonary abcess,
cutaneous and genital
amebic
lesions)."-CDC
-
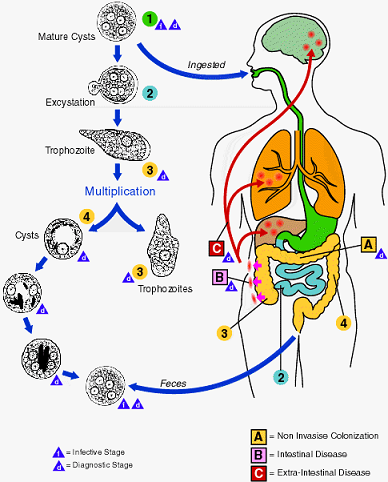
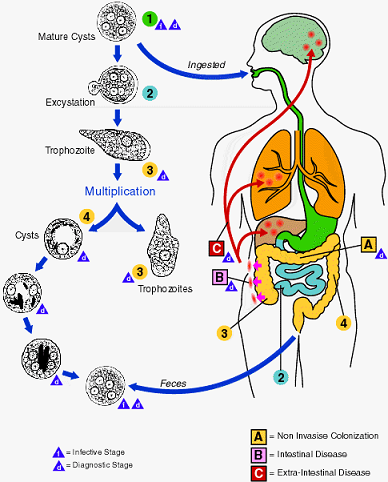
Life-cycle/Laboratory/Microscopy
-
Life Cycle
Entamoeba
histolytica
-
|
 |
-
"Infection by Entamoeba
histolytica occurs by ingestion of mature
cysts 1 in fecally contaminated food, water, or
hands.
-
Excystation
2 occurs in the small intestine and
trophozoites 3 are released,
which migrate to the large intestine. The
trophozoites multiply by binary fission and
produce cysts 4 , which are
passed in the feces.
-
Because of the protection
conferred by their walls, the cysts can survive
days to weeks in the external environment and are
responsible for transmission.
-
(Trophozoites can also be
passed in diarrheal stools, but are
rapidly destroyed once outside the body,
and if ingested would not survive
exposure to the gastric environment.)
-
In many cases, the
trophozoites remain confined to the
intestinal lumen ( A: non-invasive infection) of
individuals who are thus asymptomatic
carriers and cysts passers. In some
patients the trophozoites invade the
intestinal mucosa ( B: intestinal disease), or,
through the bloodstream, extraintestinal
sites such as the liver, brain, and lungs
( C: extra-intestinal disease),
with resultant pathologic manifestations.
It has been established that the invasive
and noninvasive forms represent separate
species, respectively E. histolytica
and E. disparindistinguishable.
-
Transmission can , which are
morphologically also occur through fecal exposure
during sexual contact (in which case not only
cysts, but also trophozoites could prove
infective)."
-
Courtesy of the Division of
Parasitic Diseases at the National Center for
Infectious Diseases, Centers for Disease Control
and Prevension (public domain)
|
-
Laboratory
Diagnosis
-
Entamoeba
histolytica must be differentiated from other
intestinal protozoa such as the nonpathogenic
amebas E. coli, E. hartmanni, E. polecki, E.
gingivalis, Endolimax nana, and Iodamoeba
bŁtschlii, and from the possibly pathogenic
Dientamoeba fragilis (which is not an ameba
but a flagellate).
-
Differentiation
is possible (but not always easy) based on
morphologic characteristics of the cysts and
trophozoites. The nonpathogenic Entamoeba
dispar, however, is morphologically identical
to E. histolytica, and differentiation
must be based on isoenzymatic, immunologic, or
molecular analysis.
-
Microscopic
identification of cysts and trophozoites in the
stool is the common method for diagnosing E.
histolytica. This can be accomplished
using:
-
Fresh stool: wet mounts and
permanently stained preparations (e.g.
trichrome). Concentrates from fresh stool:
-
wet mounts, with or without
iodine stain, and permanently stained
preparations (e.g. trichrome).
Concentration procedures, however, are
not useful for demonstrating
trophozoites.
-
In addition, E.
histolytica trophozoites can also be
identified in aspirates or biopsy samples
obtained during colonoscopy or surgery.
-
Microscopy 1: Trophozoites
of Entamoeba histolytica/dispar
-
Microscopy 2:
Trophozoites
of Entamoeba histolytica/dispar
with ingested
erythrocytes
-
Microscopy3: Cysts
of Entamoeba histolytica/dispar
Primary
Reference: Goldsmith, R. S.,
Antiprotozoal Drugs in Basic and Clinical Pharmacology (Katzung, B. G., ed) Appleton-Lange, 1998, p. 838-861.
Primary
Reference: Morgan, Juliette and
del Rio, Carlos, Amebiasis in Medicine for the Practicing
Physician (Hurst, J. W., ed) Appleton-Lange, 1996, pp.
457-459.
|