|
press  above to
begin the lecture above to
begin the lecture
return to Pharmacology Table
of Contents
Table of
Contents
- ANS
Anatomy
- Autonomic and Somatic Innervation
- Autonomic
Reflex Arc
- Autonomic Reflex Arc: First Link
- Sensory
Fiber Neurotransmitter(s)
- Autonomic Nervous System
Neurotransmitters: Summary
- CNS and the Autonomic Nervous System
- Spinal Cord Reflexes
- Hypothalamus and Nucleus tractus
solitarii
- Higher
Centers
- Peripheral ANS Divisions
- Comparison
between Sympathetic & Parasympathetic Systems
- Sympathetic
Nervous System Anatomy
- Diagram Sympathetic System
- Anatomical
Outline
- Paravertebral Ganglia
- Prevertebral Ganglia
- Terminal Ganglia
- Adrenal
Medulla
- Parasympathetic
System Anatomy
- ANS
Neurotransmitter Effector Organs
- Eye
- Heart
- Arterioles
- Systemic
Veins
- Lung
|
- Skin
- Adrenal
Medulla
- Skeletal
Muscle
- Liver
- Posterior
Pituitary
|
- Interactions
between Sympathetic & Parasympathetic Systems
- "Fight
or Flight": Characteristics of the ANS
|
- ANS
Neurotransmission
- Neurotransmitter
Criteria
- Neurotransmission Steps:
- Axonal
Conduction
- Storage
and Release of Neurotransmitter
- Combination
of Neurotransmitter and Post-Junctional
Receptors
- Termination
of Neurotransmitter Action
- Other
Non-electrogenic Functions
- Cholinergic
Neurotransmission
- Transmitter
Synthesis and Degradation
- Acetylcholinesterase
- Acetylcholine:
Storage and Release
- Site
Differences:
- Skeletal
Muscle
- Autonomic
Effectors
- Autonomic
Ganglia
- Blood
vessels
- Signal Transduction: Receptors
- Adrenergic
Transmitters: Biosynthetic Pathways
- Adrenergic
Neurotransmission: Introduction to the
Neurotransmitters
- Catecholamine
Synthesis, Storage, Release and Reuptake
- Enzymes
- Catecholamine
storage
- Regulation
of adrenal medullary
catecholamine levels
- Reuptake
- Metabolic
Transformation
- Indirect-acting
sympathomimetics
- Release
- Adrenergic
Receptor Subtypes
- ß-adrenergic
receptors
- Alpha-adrenergic
receptors
- Catecholamine
Refractoriness
- Other
Autonomic Neurotransmitters
- Co-transmission
- ATP
- VIP
- Neuropeptide
Y family
- Purines
- Nitric
Oxide
(Modulator)
- Predominant
Sympathetic/Parasympathetic Tone
- Baroreceptor
Reflexes
- Pharmacological
Modification of Autonomic Function
- Autonomic
Dysfunction
|
Sympathetic Nervous System
Anatomical Outline
- Cell bodies of
preganglionic fibers: found in intermediolateral
columns of the spinal cord (first thoracic to
second or third lumbar segments
- Preganglionic
fiber axons synapse with sympathetic ganglionic
neurons which lie outside the cerebrospinal axis.
- Sympathetic
ganglia are found at three sites:
- Paravertebral
- Prevertebral
- Terminal
- Paraverebral ganglia: 22 interconnected
pairs on either sides of the vertebral
column. (para: Gr: at the side or along side)
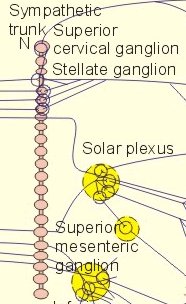 - Myelinated
preganglionic fibers (white rami:
thoracolumbar outflow only) leave
through the anterior spinal roots.
- Postganglionic
fibers (gray rami) runs back to
spinal nerves for distribution to:
- blood vessesls of
the skin
- blood vessels of
skeletal muscle
- sweat glands
- pilomotor muscles
-
Prevertebral Ganglia: abdominal and
pelvic location, comprised of:
- celiac
ganglia
- superior
mesenteric ganglia
- aorticorenal
and inferior mesenteric ganglia
-
Terminal Ganglia: few, residing near
the innervated organ, including
- ganglia
associated with the urinary bladder
and rectum
- cervical
ganglia (neck): three ganglia
(chain) mediating vasomotor,
secretory, pupillodilatory and
pilomotor responses of the head and
neck)
- All
postganglionic fibers arise from cell
bodies located within these ganglia;
the preganglionic fibers come from
upper thoracic segments: No
sympathetic preganglionic fibers come
from above the first thoracic level
-
Adrenal medulla is similar to
sympathetic ganglia.
- Difference:
- Epinephrine
is released (post-ganglionic
sympathetic fibers release norepinephrine)
- Chromaffin
cells are innerved by preganglionic fibers
that release acetylcholine.
Lefkowitz, R.J, Hoffman, B.B and
Taylor, P. Neurotrasmission: The Autonomic and Somatic
Motor Nervous Systems, In, Goodman and Gillman's The
Pharmacologial Basis of Therapeutics, (Hardman, J.G, Limbird, L.E,
Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) TheMcGraw-Hill Companies, Inc.,1996,
pp.105-107.
|
ANS
Neurotransmitters: Effector Organs
Eye
| |
|
Adrenergic
|
Effects
|
|
Cholinergic |
| Iris: Radial Muscle |
N.E., alpha-1 receptor |
contraction
(mydriasis) |
-----
|
| Iris: Sphincter muscle |
-----
|
-----
|
contraction (miosis) |
| Ciliary Muscle |
N.E., beta2 receptor |
relaxation (far vision) |
contraction (near vision) |
Heart
| |
|
Adrenergic
|
Effects
|
|
Cholinergic |
| Sino-atrial (SA) Node |
beta1; beta2 |
increase rate |
decrease rate (vagal) |
| Atrial muscle |
beta1, beta2 |
increased: contractility, conduction
velocity |
decreased: contractility, action
potential duration |
| Atrio-ventricular (AV) node |
beta1, beta2 |
increased: automaticity*,
conduction velocity |
decreased conduction velocity; AV
block |
| His-Purkinje System |
beta1, beta2 |
increased: automaticity,
conduction velocity |
------
|
| Ventricles |
beta1, beta2 |
increased: contractility,
conduction velocity, automaticity,
ectopic pacemaker |
small decrease in contractility |
-
*An increase in the slope
of phase 4 depolarization results in ENHANCED AUTOMATICITY.
-
As
a result of the increase in phase 4 slope the
cell reaches threshold more often, with a higher
heart rate as a result.
Factors that increase phase
4 depolarization include
| mechanical stretch |
beta-adrenergic stimulation |
hypokalemia |
- Ischemia
can induce abnormal automaticity, i.e.
automaticity that occurs in cells not typically
exhibiting pacemaker activity.
- Acetylcholine is
an example of an agent that decreases the
slope of phase 4 depolarization and as a
result, slows the heart rate.
Arterioles
| |
Adrenergic
|
Effects
|
Cholinergic |
| Coronary |
alpha 1, 2; beta2 |
constriction;dilatation |
constriction |
| Skin/Mucosa |
alpha 1, 2 |
constriction |
dilatation |
| Skeletal Muscle |
alpha; beta2 |
constriction,dilatation |
dilatation |
| Cerebral |
alpha1 |
slight constriction |
dilatation |
| Pulmonary |
alpha1, beta2 |
constriction; dilatation |
dilatation |
| Abdominal viscera |
alpha1, beta2 |
constriction; dilatation |
------- |
| Salivary glands |
alpha1,2 |
constriction |
dilatation |
| Renal |
alpha 1, 2;beta1,2 |
constriction;dilatation |
--------- |
Systemic
Veins
| |
|
Adrenergic
Effects
|
Cholinergic |
| systemic veins |
alpha1,2; beta2 |
constriction; dilatation |
-----
|
Lung
| |
|
|
Adrenergic
Effects
|
Cholinergic |
| Tracheal and bronchial muscle |
beta2 |
Relaxation |
contraction |
| Bronchial glands |
alpha1, beta2 |
decrease secretion; increased secretion |
stimulation |
Kidney
| |
|
Adrenergic
Effects
|
Cholinergic |
| Renin Secretion |
alpha1; beta1 |
decrease; increase |
------- |
Skin
| |
|
Adrenergic
Effects
|
Cholinergic |
| Pilomotor muscles |
alpha1 |
contraction |
----- |
| Sweat glands |
alpha1 |
localized secretion |
generalized secretion |
Adrenal
Medulla
| |
Adrenergic
Effects
|
Cholinergic |
| Adrenal medulla |
-- |
---- |
Secretion of epinephrine and
norepinephrine (mainly nicotinic and some muscarinic) |
Skeletal
Muscle
| |
|
Adrenergic
Effects
|
Cholinergic |
|
Skeletal Muscle
|
beta2 |
increased: contractility;
glycogenolysis; potassium uptake |
---------- |
Liver
| |
|
Adrenergic
Effects
|
Cholinergic |
| Liver |
alpha1;beta 2 |
glycogenolysis and
gluconeogenesis |
-------- |
Posterior Pituitary
| |
|
|
Adrenergic
Effects
|
Cholinergic |
| Posterior Pituitary |
beta 1 |
Antidiuretic hormone secretion
(ADH) |
------------ |
Based on Table
6-1: Lefkowitz, R.J, Hoffman, B.B and Taylor, P.
Neurotransmission: The Autonomic and Somatic Motor
Nervous Systems, In, Goodman and Gillman's The
Pharmacologial Basis of Therapeutics, (Hardman, J.G, Limbird, L.E,
Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) TheMcGraw-Hill Companies, Inc.,1996,
pp.110-111
Characteristics of Autonomic
Organ Innervation
Examples of Antagonistic Interactions
between Sympathetic and Parasympathetic Systems
|
|
|
Interdependent or Complementary
Sympathetic and Parasympathetic Effects
- Actions of
sympathetic and parasympathetic systems on male
sexual organs are complementary.
|
Independent Effects
- Vascular
resistance is mainly controlled by sympathetic
tone.
|
|
Fight
or Flight: General Functions of the Autonomic Nervous System
ANS
regulates organs/processes not under conscious
control including:
circulation
|
digestion
|
respiration
|
temperature
|
sweating
|
metabolism
|
some
endocrine gland secretions
|
| temperature
regulation |
regulation
of glucose levels |
rapid
vascular response to hemorrhage |
reacting
to oxygen deficiency
|
Sympathetic
Responses
| heart rate increases |
blood pressure
increases
|
blood is shunted to
skeletal muscles
|
blood glucose
increase
|
bronchioles dilate
|
pupils dilate
|
| many
of these effects are primarily due to or
augmented by epinephrine release from the adrenal
medulla |
Parasympathetic
responses
| slows heart rate |
lowers blood
pressure |
increases
gastrointestinal motility |
| protects retina
from excessive light |
empties the bowel
and bladder |
promotes
absorption of nutrients |
Lefkowitz, R.J, Hoffman, B.B and Taylor, P.
Neurotrasmission: The Autonomic and Somatic Motor Nervous Systems, In,
Goodman and Gillman's The Pharmacologial Basis of Therapeutics,
(Hardman, J.G, Limbird, L.E, Molinoff, P.B., Ruddon, R.W, and Gilman,
A.G.,eds) TheMcGraw-Hill Companies, Inc.,1996, pp.108..
|
press the purple
arrow below (right) to go to the next page
|