|
Pharmacokinetics: Ketamine (Ketalar),
Etomidate (Amidate)
|
Ketamine (Ketalar) |
Phencyclidine |
Phencyclidine
1-(1-Phenylcyclohexyl)piperidine;
C17H25N |
-
Ketamine (Ketalar) pharmacology-- a summary of organ system and other effects:5
-
CNS action: Ketamine (Ketalar) induces a unique
anesthetic state referred to as dissociative anesthesia in which
the patient may appear "awake" or as is frequently
described "cataleptic". Specific characteristics:
Significant analgesia-- subanesthetic doses still
provide analgesia; Eyes remain open with cough, swallow, and
corneal reflexes present; Amnestic properties are present but less
than that observed with benzodiazepines, e.g. midazolam (Versed)
-
Anesthesia induction characteristics:
-
increased limb muscle tone
-
salivation, lacrimation, nystagmus,
pupillary dilatation
-
CNS metabolic effects: increased metabolism,
blood flow, and intracranial pressure
-
Increased electroencephalographic activity
-
Emergence syndrome: There is a significant
likelihood (10%-30%) that the patient will experience unusual
psychological reactions to ketamine (Ketalar)
anesthesia. These reactions include
illusions/hallucinations and "out of body"
experiences-- collectively termed emergence syndromes which
may last 1-3 hours.
-
Pulmonary effects -- very limited. Limited
pulmonary effects apply when ketamine (Ketalar) is used as the
only agent; however, respiratory depression would occur in
ketamine (Ketalar) is combined with other drugs which are
classified as CNS depressants.
-
Ketamine (Ketalar) tends to relax bronchial
smooth muscle
-
Salivation following ketamine (Ketalar)
administration may trigger laryngospasm.
Furthermore, despite retention of reflexes, aspiration may
still occur
-
Cardiovascular effects: The stimulant
characteristics of ketamine (Ketalar) are manifest in
cardiovascular responses that seem opposite to that observance
most anesthetics.
-
For example, ketamine (Ketalar)
administration increases heart rate, cardiac output, and blood
pressure.
-
These effects may be relatively contraindicated in
patients sensitive to the expectable increase in myocardial oxygen
consumption.
-
Drugs can reduce these positive chronotropic
and hypertensive effects. Examples of drugs which can reduce
these cardiovascular effects include benzodiazepines, barbiturates
and adrenergic receptor blockers. The centrally acting and
hypertensive agents such as clonidine (Catapres) would also be
affected by reducing central sympathetic outflow.
-
Overview: Etomidate (Amidate):
5,6
-
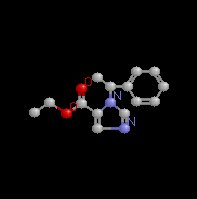
Etomidate (Amidate) which chemically is a carboxylated imidazole
derivative is an effective IV anesthetic agent which exhibits
favorable hemodynamic properties with minimal respiratory
depression.
-
This drug produces rapid unconsciousness (within about 30
seconds) following IV administration. The patient will
recover quickly with awakening being more rapid than with
barbiturates, not including propofol (Diprivan).
-
Adverse effects, however, have resulted in reduced clinical
use.
-
These adverse effects have included injection site pain
(which may be prevented by local anesthetic preinjection),
thrombophlebitis, myoclonus, nausea and vomiting, and inhibition
of steroid synthesis.
-
Nausea and vomiting may be especially
associated with etomidate (Amidate) compared to other induction
drugs and is made worse by concurrent use of opioids. This
problem might be managed by avoiding etomidate (Amidate) in those
patients with a known history of postoperative nausea or by
pre-treatment with antinausea medication.
-
Etomidate (Amidate), a water insoluble drug which must be
dissolved in propylene glycol {35%; pH 6.9} has a chiral carbon,
resulting into enantiomers (stereoisomers) of which only one
enantiomer is active.
Etomidate
|
 |
-
Etomidate (Amidate)
pharmacokinetics:
5,6
-
Metabolism: Etomidate (Amidate) is metabolized by ester
hydrolysis (hepatic & tissue) as well as N-dealkylation.
Metabolites are inactive and excreted by renal and biliary routes.
-
Etomidate (Amidate) administration results in rapid onset,
follow by an initial redistribution phase which is also rapid
(initial redistribution halftime = 2.7 minutes). Analysis of the
concentration-decay curve suggests that a three-compartment model
best fits the observed time dependent drop in plasma etomidate (Amidate)
concentration. However, the initial rapid redistribution
time is most pertinent for explaining the observed rapid recovery
following IV administration.
-
Etomidate (Amidate) clearance ranges from 18-25 ml/kg/min.
(compared to, for example thiopental (Pentothal) which is a
clearance of about 3.5 ml/kg/min.
-
Vd is large, consistent with a relatively lipophilic
compound which gains access to many compartments.
-
Rapid onset following IV administration is typical it has been
described as "one arm-brain circulation time".
Infusion noses about 10 μg/kg/minute with etomidate (Amidate)
administered often in combination with an opioid.
-
Etomidate (Amidate) pharmacology-- a summary of organ system and other effects:
5,6
-
CNS: Similar to observations concerning
thiopental (Pentothal) and other barbiturates, etomidate (Amidate)
while producing hypnosis does not produce analgesia. Also
similar to the barbiturates, etomidate (Amidate) may function by
interacting with GABA receptor systems.
-
Cerebral metabolism is reduced as well a
cerebral blood flow following etomidate (Amidate); these
effects result in a more favorable cerebral oxygen supply over
demand ratio. Also intracranial pressure (ICP) is
reduced by etomidate (Amidate); moreover, further ICP
reduction is available by reducing PaCO2.
-
Activation of the EEG following the etomidate (Amidate)has been observed and this property may be the basis
for epileptogenic activity. Perhaps also related is the
observation that about 50% of patients receiving etomidate (Amidate)
will exhibit myoclonus (spontaneous movements).
-
Pulmonary:
-
Ventilation is depressed less
with etomidate (Amidate) compared to barbiturates, but apnea may
follow from rapid IV etomidate (Amidate) administration.
-
Importantly, given that etomidate (Amidate) may be administered
concommittantly with an opioid (or inhaled anesthetic),
respiratory depression can occur as a result of these
combinations.
-
Cardiovascular: An important distinction between
etomidate (Amidate) and other induction agents is that etomidate (Amidate)
has very minimal cardiovascular effects.
-
Furthermore, during
induction blood flow to the heart and oxygen consumption are both
reduced which allows maintenance of the balance between oxygen
supply and requirement.
-
Since etomidate (Amidate) does not alter
sympathetic or baroreceptor reflex function, undesirable
hemodynamic effects may be induced by intubation.
-
Accordingly, an opioid (perhaps fentanyl (Sublimaze)), as
noted above, maybe given along with etomidate (Amidate).
-
Endocrine: Etomidate (Amidate) will cause
postoperative suppression of adrenocortical function.
-
This
effect occurs because etomidate inhibits 11-ß-hydroxylase and
17-α-hydroxylase enzymes which are important in cortisol
synthesis.
-
Short-term adrenocortical suppression as
might occur following single induction doses is not thought to
be clinically serious.
|