Medical Pharmacology Chapter 35 Antibacterial Drugs
First Generation Cephalosporins
|
Cefazolin Introduction
Cefazolin stands as a classical first-generation cephalosporin antibiotic that has maintained its clinical prominence since its synthesis in 1967, and is considered a foundational drug in contemporary infectious disease therapy and perioperative prophylaxis.2
Cefazolin Mechanism of Action and Bacteriocidal Activity
Cefazolin exerts its antimicrobial effect through a well-characterized mechanism of bacterial cell wall inhibition.3,4
Similar to all beta-lactam antibiotics, cefazolin possesses a four-membered beta-lactam ring structure that enables it to function as a structural analog of the D-alanine-D-alanine motif present in bacterial peptidoglycans.
The drug binds covalently to penicillin-binding proteins (PBPs), which are bacterial transpeptidases responsible for catalyzing the formation of isopeptide cross-linkages between peptidoglycan strands, the terminal step in bacterial cell wall synthesis.
By inhibiting this critical transpeptidation reaction, cefazolin prevents the cross-linking of peptidoglycan polymers, resulting in structural instability and weakness of the bacterial cell wall.
This destabilization triggers autolytic degradation of the cell wall, as bacteria continuously remodel their peptidoglycan matrix during growth and cell division.
![]() The
consequence is bacterial cell lysis and death, making
cefazolin bactericidal rather than merely bacteriostatic.
The
consequence is bacterial cell lysis and death, making
cefazolin bactericidal rather than merely bacteriostatic.
Cefazolin demonstrates superior in vitro bactericidal activity compared to other first-generation cephalosporins such as cephalexin, with particularly enhanced potency against gram-negative organisms such as Escherichia coli and Klebsiella pneumoniae, where it demonstrates two to eightfold greater activity.2,5
![]() Cefazolin Spectrum of Activity
Cefazolin Spectrum of Activity
Introduction
The spectrum of activity of cefazolin encompasses primarily gram-positive organisms, particularly streptococci species and methicillin-susceptible Staphylococcus aureus (MSSA), resulting in its efficacy against the most common pathogens encountered in skin and soft tissue, bone and joint, and urinary tract infections.6,7,8
The drug also demonstrates moderate but clinically useful activity against select gram-negative organisms including E. coli, Klebsiella pneumoniae, and Proteus mirabilis.
![]() Cefazolin is ineffective against methicillin-resistant Staphylococcus aureus (MRSA), which possess the mecA
gene encoding penicillin-binding protein 2A (PBP2A), a
low-affinity PBP that does not effectively bind beta-lactam
antibiotics.
Cefazolin is ineffective against methicillin-resistant Staphylococcus aureus (MRSA), which possess the mecA
gene encoding penicillin-binding protein 2A (PBP2A), a
low-affinity PBP that does not effectively bind beta-lactam
antibiotics.
Cefazolin lacks activity against enterococci, anaerobic organisms, and most Enterobacteriaceae that produce extended-spectrum beta-lactamases.
![]() Gram-Positive Coverage
Gram-Positive Coverage
A therapeutic strong point of cefazolin is its excellent activity against Gram-positive organisms. Cefazolin may be the beta-lactam antibiotic of choice for MSSA infections in patients who can tolerate cephalosporins but not penicillins.
Staphylococcus aureus (Methicillin-Susceptible-MSSA)32,33
Cefazolin is highly active against MSSA.
This agent may be preferred over anti-staphylococcal penicillins (e.g., nafcillin, oxacillin) for non-CNS infections due to a superior safety profile and more convenient dosing schedule, while maintaining equivalent efficacy.
The mechanism of susceptibility relies on the accessibility and affinity of the native PBPs.
Coagulase-Negative Staphylococci (CoNS)
Cefazolin is active against methicillin-susceptible strains (e.g., S. epidermidis, S. lugdunensis).
Rates of methicillin resistance (mediated by mecA) are generally higher in community and hospital isolates of CoNS than for S. aureus.34
Streptococci: Cefazolin exhibits excellent activity against beta-hemolytic streptococci35
Streptococcus pyrogenes (Group A Strep)
Streptococcus agalactiae (Group B Strep)
Streptococcus dysgalactiae
Viridans Group Streptococci36
Cefazolin is active against most strains, making it a viable option for endocarditis caused by these organisms, though penicillin-resistant strains may show reduced susceptibility.
Streptococcus pneumoniae37
Active against penicillin-susceptible isolates.
Penicillin-resistant pneumococci often have altered PBPs that confer cross-resistance to first-generation cephalosporins.
Cefazolin should not be relied upon for meningitis or severe pneumococcal pneumonia where resistance is suspected.
Cefazolin Pharmacokinetics and Distribution9,10
Cefazolin is administered exclusively via parenteral routes, intravenously or intramuscularly, given its limited gastrointestinal bioavailability.
Oral administration does not reliably result in therapeutic levels.
Cefazolin following intravenous administration is rapidly distributed.
Distribution half-life is about 4 minutes.
Peak plasma concentrations are achieved rapidly following bolus injection, providing immediate bactericidal activity at tissue sites.
Volume of distribution is approximately 0.2 to 0.25 liters per kilogram, indicating confined distribution consistent with a hydrophilic molecule that does not extensively penetrate lipid-rich compartments.
An important pharmacokinetic property of cefazolin is its high degree of protein binding in serum, which approaches 80 percent.9,11
This extent protein binding has critical implications for pharmacodynamic efficacy as only the unbound drug fraction possesses antimicrobial activity.
Protein binding of cefazolin demonstrates concentration-dependent characteristics as higher drug concentrations result in relatively decreased protein binding which may lead to higher unbound drug fractions at elevated doses.
In interstitial fluid accumulating within tissue-embedded spaces, approximately 30% of cefazolin remains protein-bound, compared to 80% in serum, resulting in significantly higher free drug concentrations at tissue sites.
Elimination of cefazolin occurs primarily through renal excretion, with the drug being cleared predominantly by glomerular filtration, supplemented by active tubular secretion.10,12,13
Serum elimination half-life in patients with normal renal function is approximately 1.5 to 2 hours, though more recent population pharmacokinetic studies suggest a terminal half-life of approximately 57.93 minutes.
In anephric patients (those without renal function), the serum half-life extends dramatically to approximately 42 hours.
Total elimination constant and renal clearance of cefazolin vary linearly with creatinine clearance, indicating that as renal function declines, drug accumulation becomes proportionally significant.12,14
More than 90 percent of an administered dose is recovered in the urine of patients with normal renal function during the first 24 hours.
Peak urine levels range from 60 to over 2,000 micrograms per milliliter, reflecting the renal concentration process.
Cefazolin is not significantly metabolized by hepatic enzymes.15
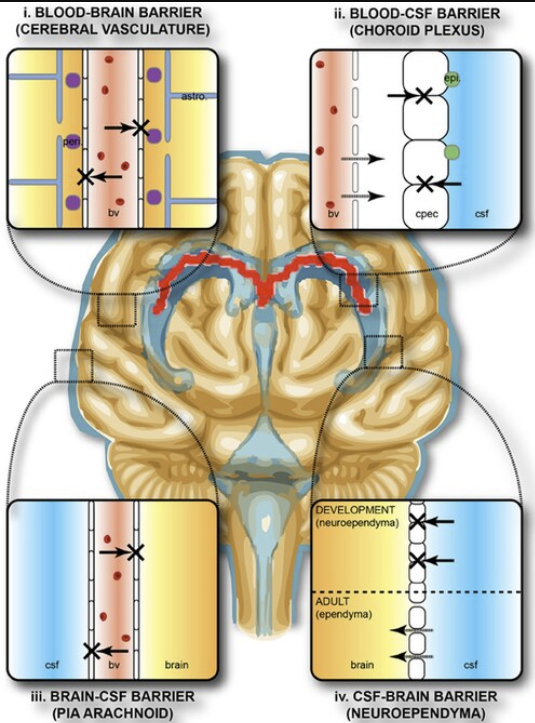
Cefazolin does not cross the blood-brain barrier to a clinically useful extent under normal circumstances, with cerebrospinal fluid (CSF) penetration being limited in the absence of meningeal inflammation.16
Tissue Penetration and Compartment-Specific Pharmacokinetics
![]() Cefazolin
is especially important in perioperative prophylaxis.8,17,18
Cefazolin
is especially important in perioperative prophylaxis.8,17,18
Bone tissue achieves particularly high concentrations of cefazolin, with peak bone concentrations occurring approximately 40 minutes after parenteral administration, with a bone tissue half-life of approximately 42 minutes compared to the serum half-life of 108 minutes.
Favorable bone penetration reflects the drug's hydrophilicity and its ability to accumulate in mineralized tissue through multiple mechanisms.
Recent pharmacokinetic studies indicates that optimal bone and soft tissue concentrations are achieved when cefazolin is administered between 10 and 30 minutes before tourniquet inflation during orthopedic procedures.
Median bone concentration-to-serum concentration ratio is approximately 0.25, with a reported range of 0.06 to 0.41.
In continuous infusion studies of cefazolin for bone and joint infections, median bone concentrations reached 13.5 micrograms per gram, with considerable individual variation.
![]() The
blood-brain barrier presents a significant limitation to
cefazolin distribution in the absence of meningeal
inflammation.10
The
blood-brain barrier presents a significant limitation to
cefazolin distribution in the absence of meningeal
inflammation.10
 |
|
Until recently, cefazolin penetration into cerebrospinal fluid was thought prohibitively low.
Contemporary evidence suggests more nuanced penetration patterns.19
![]() Even
in the absence of meningeal inflammation, the
cerebrospinal fluid distribution ratio of cefazolin
may be approximately 3 to 5 percent of serum
concentrations, which may nevertheless achieve
therapeutic concentrations in certain clinical
scenarios.
Even
in the absence of meningeal inflammation, the
cerebrospinal fluid distribution ratio of cefazolin
may be approximately 3 to 5 percent of serum
concentrations, which may nevertheless achieve
therapeutic concentrations in certain clinical
scenarios.
When meningeal inflammation is present, as occurs during meningitis or ventriculitis, the blood-brain barrier becomes more permeable, and CSF penetration improves substantially, potentially allowing therapeutic concentrations to be achieved.
Despite this finding, cefazolin is typically not considered a first-line agent for bacterial meningitis due to its generally limited CNS penetration, particularly in the prophylaxis or treatment of central nervous system infections in immunocompetent individuals.
|
Parameter |
Value |
Clinical Implication |
|
Bioavailability |
Not applicable (parenteral administration) |
Requires IV or IM administration |
|
Protein Binding |
74%-86%23 |
High binding; only free drug is active; drug interacts with albumin levels. |
|
Half-life (t1/2) |
1.8-2.0 hours22 |
Allows q8h dosing |
|
Volume of Distribution (Vd) |
0.19 L/kg22 |
Drug mostly localized to the extracellular domain. Effective for blood/soft tissue infections |
|
Excretion |
Renal (as unchanged drug)23 |
Requires dose adjustment if renal failure present; effective agent for urinary tract infections. |
|
CSF Penetration |
<4%23 |
Contraindicated for treating meningitis |
Cefazolin Pharmacodynamics and Time-Dependent Antimicrobial Activity
Optimal cefazolin utilization depends on its pharmacodynamic
profile.20,21
Unlike aminoglycosides, which demonstrate
concentration-dependent killing, increasing the peak serum
concentration of cefazolin beyond four times the minimum
inhibitory concentration does not enhance bactericidal
activity. Instead, increasing the concentration only results
in enhanced adverse effect risk.
Population pharmacokinetic analyses suggest that continuous
infusion of cefazolin is associated with improved target
attainment compared to bolus dosing.20
![]() Cephalosporins,
including cefazolin, exhibit time-dependent bactericidal
activity, meaning that antimicrobial efficacy is determined
primarily by the proportion of the dosing interval during
which unbound drug concentrations remain above the minimum
inhibitory concentration (T>MIC) of the target pathogen.
Cephalosporins,
including cefazolin, exhibit time-dependent bactericidal
activity, meaning that antimicrobial efficacy is determined
primarily by the proportion of the dosing interval during
which unbound drug concentrations remain above the minimum
inhibitory concentration (T>MIC) of the target pathogen.
![]() This
pharmacodynamic principle effects dosing strategy, as
extended infusions or continuous infusions of cefazolin may
optimize T>MIC and potentially improve clinical outcomes
compared to standard bolus administration.21
This
pharmacodynamic principle effects dosing strategy, as
extended infusions or continuous infusions of cefazolin may
optimize T>MIC and potentially improve clinical outcomes
compared to standard bolus administration.21
In summary, for cephalosporins, maximizing the time above MIC is critical.
The goal is typically to maintain free drug levels above the MIC for at least 50-60% of the dosing interval for bactericidal activity.
For serious infections (like endocarditis) or in neutropenic hosts, 100% T > MIC is often targeted to limit the likelihood of regrowth.
High peaks and 1.8-hour half-life of cefazolin facilitate achieving these targets with q8h dosing for most systemic infections, whereas continuous infusion strategies are sometimes employed for critical cases.22
Cefazolin Mechanisms of Resistance
Although cefazolin is very useful clinically, bacteria have evolved mechanisms to evade its action.
Beta-Lactamase Production
The most frequently encountered resistance mechanism in Staphylococci and Gram-negatives is production of beta-lactamases, enzymes that hydrolyze the beta-lactam ring.
Staphylococcal Beta-Lactamases (BlaZ) and the Inoculum Effect
Most S. aureus strains (>90%) produce penicillinase (BlaZ), rendering them resistant to penicillin.
Cefazolin was specifically designed to resist hydrolysis by this enzyme.
However, BlaZ exists in different serotypes (A, B, C, D) with varying kinetic properties.
The Cefazolin Inoculum Effect (CIE)24
A phenomenon known as the Cefazolin Inoculum Effect is observed when the MIC of the drug rises significantly (often >4-fold or crossing the susceptibility breakpoint) when the bacterial inoculum is increased from the standard 105 CFU/mL to a high density of 107 CFU/mL (mimicking deep abscesses or cardiac vegetations). [CFU/mL + Colony Forming Units per milliliter]
Mechanism25,26,27
Some MSSA strains produce Type A BlaZ, which has a higher catalytic efficiency for hydrolyzing cefazolin compared to Type C variants.
![]() While cefazolin is generally stable against staphylococcal
beta-lactamases at standard densities, the massive amount of
Type A enzyme present in a dense infection can degrade the
drug locally, potentially leading to therapeutic failure.
While cefazolin is generally stable against staphylococcal
beta-lactamases at standard densities, the massive amount of
Type A enzyme present in a dense infection can degrade the
drug locally, potentially leading to therapeutic failure.
Prevalence
Type A BlaZ is found in 15%-40% of clinical MSSA isolates.
Clinical Relevance
Clinical impact of the CIE remains debatable and appears to be mainly a concern in high-burden infections like endocarditis.
Gram-Negative Beta-Lactamases
TEM-1 and SHV-1
These are common plasmid-mediated beta-lactamases found in E. coli and K. pneumoniae.
TEM-1 BETA-Lactamase is the most common plasma-encoded beta-lactamase and is responsible for most of ampicillin resistance in bacteria.
This beta-lactamase is named after an Athenian patient, Temoriera, from whom the first isolate was obtained.
In excess of 170 variance have evolved.28
Cefazolin is relatively stable to these narrow-spectrum enzymes compared to ampicillin, but hyper-production can lead to resistance.
ESBLs (Extended-Spectrum Beta-Lactamases)
Enzymes like CTX-M, TEM-10, and SHV-12 hydrolyze broad-spectrum cephalosporins (ceftriaxone) and cefazolin.29
AmpC Beta-lactamases
Organisms like Enterobacter and Serratia carry chromosomal AmpC.30
Cefazolin is a strong inducer of AmpC expression and is rapidly hydrolyzed by it.
Cefazolin should not be used for organisms known to harbor inducible AmpC, as it can select for de-repressed mutants during therapy.
Cefazolin at low concentrations induce AmpC gene expression.
This gene induction results in high levels of the AmpC enzyme which can rapidly hydrolyze many Beta-lactams (such as cefazolin and other cephalosporins).
Even if the bacteria appear susceptible to cefazolin initially, clinical resistance develops rapidly during treatment.
Altered Penicillin-Binding Proteins
Changes in penicillin-binding proteins represent the mechanism of cefazolin resistance in MRSA and Penicillin-Resistant Streptococcus pneumoniae.
In MRSA, the acquisition of the mecA gene leads to the production of PBP2a.
Cefazolin cannot bind effectively to PBP2a, rendering the bacteria resistant.
This mechanism is an intrinsic resistance mechanism.
Therefore, increasing the dose of cefazolin will not overcome PBP2a-mediated resistance.31
Porin Channel Mutations39
In Gram-negative bacteria like E. coli and P. mirabilis, beta-lactams must diffuse through outer membrane porin channels to reach the PBPs in the periplasmic space.
Mutations that downregulate porin expression (for example, OmpF/OmpC loss) reduce the intracellular concentration of the drug.38
This mechanism often works in concert with beta-lactamase production to confer high-level resistance.
November-December 2025
|
|
|
|
This Web-based pharmacology and disease-based integrated teaching site is based on reference materials, that are believed reliable and consistent with standards accepted at the time of development. Possibility of human error and on-going research and development in medical sciences do not allow assurance that the information contained herein is in every respect accurate or complete. Users should confirm the information contained herein with other sources. This site should only be considered as a teaching aid for undergraduate and graduate biomedical education and is intended only as a teaching site. Information contained here should not be used for patient management and should not be used as a substitute for consultation with practicing medical professionals. Users of this website should check the product information sheet included in the package of any drug they plan to administer to be certain that the information contained in this site is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. Advertisements that appear on this site are not reviewed for content accuracy and it is the responsibility of users of this website to make individual assessments concerning this information. Medical or other information thus obtained should not be used as a substitute for consultation with practicing medical or scientific or other professionals. |