Chapter 10: Pharmacological Management of Congestive Heart Failure
|
See description below, also.
|
Figures from "Harrison's Principles of Internal Medicine", Thirteenth Edition, pages 995 and 996.
|
|
Drugs used in heart failure include those used to initially manage mild to moderate failure and those used more commonly in severe to very severe conditions.
First Agents Used:
ACE inhibitors
Diuretics
Cardiac Glycosides
Beta-blockers (mild-to-moderate disease)
Additional Agents:
More aggressive diuretic therapy
Vasodilators
parenteral inotropic agents (dobutamine)
Selection of agents and their combinations depend on initial clinical state and on patient responsiveness to initial therapy.
Factors Influencing Cardiac performance and Output
Ventricular end-diastolic volume (preload)
Atrial contraction
Inotropic state (myocardial contractility)
Ventricular afterload
Exercise
|
|
Ventricular end-diastolic volume (preload)
For any given inotropic state, ventricular performance will be significantly affected by the degree of ventricular stretch as determined by ventricular end-diastolic volumes (EDV).
The general relationship, as shown above, is the Frank-Starling mechanism.
Several factors influence end diastolic volumes, beginning with total blood volume.
Significant volume depletion leads to decreased cardiac output with preload and end-diastolic volumes declining.
Blood volume distribution is important. Factors that affect distribution include:
Body position: gravitational forces, in the upright individual, results in pooling to extrathoracic compartments, especially the legs.
By contrast, in the recumbent individual, blood will redistribute into the thorax, increasing preload.
Venous tone:
Venular smooth muscle tone is under sympathetic neural and humoral control.
Exercise or hypotension result in venoconstriction and an increase in intrathoracic, intraventricular blood volume.
Accordingly, these conditions increase cardiac output by increasing end-diastolic volumes.
Skeletal muscle activity: During exercise, blood is displaced from the periphery due to the squeezing action of contracting muscle on the venous bed. Increased preload results as does increased cardiac output and work.
Atrial contraction
Atrial contraction (atrial kick) enhances ventricular filling.
In the hypertrophic ventricle (with reduced compliance) appropriately time atrial contraction may be especially important in achieving adequate levels of ventricular filling.
Increase heart rate (reduced filling times) or atrial arrhythmias reduce or eliminate the effectiveness of atrial kick.
Inotropic state (myocardial contractility)
Factors that influence the inotropic state affect ventricular performance at a given ventricular end-diastolic volume. These factors change the concentration of Ca2+ at the myofilaments and include in part:
Adrenergic nerve activity: The amount of norepinephrine released by cardiac adrenergic nerve endings is the most important acute factor in changing the position of the force-velocity in ventricular function curves.
Circulating catecholamines: Catecholamines released from adrenal medulla and other non-cardiac sympathetic ganglia stimulate cardiac adrenoceptors increasing rate and force of contraction.
Exogenously administered agents:
Drugs that improve ventricular performance include:
cardiac glycosides
dopamine (Intropin)/dobutamine (Dobutrex)
caffeine
isoproterenol (Isuprel)
theophylline
calcium
Exogenously administered agents:
Drugs that decrease ventricular performance:
procainamide (Procan SR, Pronestyl-SR)
disopyramide (Norpace)
certain calcium channel blockers
barbiturates
alcohol
local and general anesthetics
Physiological Depressants:
Depression of the myocardial force-velocity curves with decreased left ventricular function can occur with hypoxia, hypercapnia, ischemia, and acidosis.
Loss of ventricular muscle mass effects occur when significant portions of the ventricular are hypokinetic or necrotic either due to ischemia or following myocardial infarction.Total ventricular performance may be significantly depressed.
Ventricular afterload
Afterload is the stress developed in the wall of the ventricle during ejection and depends on aortic pressure and ventricular dimensions.
Myocardial fiber tension is determined by the product of the intracavity ventricular pressure and radius divided by wall thickness (Laplace's law).
Therefore, for the same level of aortic pressure, afterload increases with ventricular dilation.
Left ventricular stroke volume is inversely proportional to afterload.
In the failing heart with limited or no preload reserve (increasing preload in a normal heart increase contractility), afterload determines ventricular performance.
When afterload increases (increase in vasoconstriction) in the failing heart, cardiac output may be reduced further even while oxygen demand increases.
Vasodilators may improve myocardial performance by reducing ventricular afterload.
With exercise, venous return is significantly increased and results in enhanced ventricular filling and preload.
Increases in cardiac adrenergic activity and increases in circulating levels of catecholamines increase heart rate and enhance the myocardial contractility.
These factors result in significantly augmented cardiac output.
Arterial pressure does not increase substantially since vasodilatation in exercising muscles offset the increase in cardiac output.
Myocardial Adaptation including Neurohumoral Adjustments
Adaptive mechanism to assist the failure heart
Frank-Starling relationship: Increasing preload leads to increased cardiac output.
Myocardial hypertrophy which tends to reduce ventricular wall tension towards normal.
Redistribution of cardiac output from skin, kidneys, and skeletal muscle to the brain and heart.
Neurohumoral adjustments which maintain arterial pressure
Renin-Angiotensin System (RAS): Activation of the RAS occurs with declining cardiac output.
Increasing concentrations of circulating angiotensin II and aldosterone results in excess vasoconstriction and salt and water retention respectively.
The clinical condition of patients with chronic heart failure may be improved by administration of aldosterone antagonists and ACE inhibitors.
Adrenergic System: Patients with heart failure often have significantly elevated circulating norepinephrine levels.
These levels provide critical inotropic support for the failing myocardium.
Administration of
![]() -adrenoceptor
antagonists to patients with
severe failure may worsen their congestive
heart failure.
-adrenoceptor
antagonists to patients with
severe failure may worsen their congestive
heart failure.
Administration of
![]() -adrenoceptor antagonists
to patients with mild to moderate failure
may be helpful in management of their
congestive heart failure.
-adrenoceptor antagonists
to patients with mild to moderate failure
may be helpful in management of their
congestive heart failure.
Congestive Heart Failure: Causes
Arrhythmias: In patients with heart disease and with a history of congestive failure, an acute arrhythmia is a common precipitating cause of CHF.
Tachyarrhythmias decrease filling time and as a result decrease cardiac output.
Since increased heart rate increases myocardial oxygen demand, cardiac ischemia may be induced which may lead to reduced contractility.
A-V dissociation results in loss of the atrial contribution to ventricular filling. Therefore end-diastolic volume is reduced with an attendant reduction in cardiac output
Abnormal intraventricular conduction may cause a reduced synchronicity of contraction with a reduction in myocardial performance.
Optimal output requires coordinated impulse propagation and contraction
Severe bradycardia in the absence of increased stroke volume can seriously reduce cardiac output and thus precipitate CHF. Increased stroke volume may not be possible if the patient has significant heart disease.
Myocardial Infarction: A myocardial infarction, reducing left ventricular function, may precipitate CHF in a previously hemodynamically compensated patient.
Pulmonary Embolism: Physically inactive patients with low cardiac output may develop deep venous thrombi which may produce pulmonary emboli and elevation of pulmonary arterial pressure. Increased pulmonary artery pressure may worsen or cause left ventricular failure.
Systemic Hypertension: Rapid increases in arterial blood pressure with associated increases in peripheral resistance can increase afterload to an extent sufficient to produce heart failure.
Other causes:
Thyrotoxicosis
Pregnancy
Infection
Anemia
Rheumatic and other forms of Myocarditis
Physical, dietary, fluid, environmental and emotional excesses
Infective Endocarditis
Reference: Isselbacher et al. (eds): "Harrison's Principles of Internal Medicine"New York, McGraw-Hill Inc, 1994, p. 999.
Clinical Use: Sympathomimetic Agents
Overview--Clinical Uses
Positive inotropic agent
increase myocardial contractility
Vasopressors
increase systemic blood-pressure after sympathetic nervous system blockade following regional anesthesia
maintenance of systemic blood-pressure during:
during elimination of excess inhaled anesthetic
during restoration of intravascular fluid volume
prolonged sympathomimetic administration to support blood-pressure is not recommended
Disadvantages associated with using sympathomimetics without significant ß1 -- adrenergic effects:
intense vasoconstriction
hypertensive responses promoting reflex-mediated bradycardia
Treatment of bronchospasm in patients with asthma
Addition to local anesthetic solutions -- reducing systemic local anesthetic absorption
Management of severe allergic (hypersensitivity) reactions
Shock: Inadequate Tissue Perfusion
Microcirculatory failure is the most critical failure in shock.
Pathological factors such as leukocyte/platelet adhesion and coagulation can result in microvessel occlusion.
Microvascular flow is affected by the balance between colloid forces (tending to retain intravascular fluid volume) and capillary hydrostatic pressure (tending to force fluid into extravacular space)
Vasoconstriction of precapillary resistance vessels reduce capillary hydrostatic pressure and vasoconstiction of postcapillary venules tend to increase hydrostatic pressure gradients.
In hypoxic states, arteriolar metabolic effects may dominate causing precapillary vasodilation and with vasoconstriction of postcapillary venules, movement of fluid into extravascular spaces is favored.
Tissue edema may be further worsened by circulating toxins which enhances capillary permeability.
Intravascular plasma protein loss decreases oncotic (colloid) forces which causes additional intravascular fluid loss.
Hypovolemic shock: Dehydration or Blood Loss
Treatment includes fluid infusion to obtain adequate cardiac preload (filling pressure) without precipitating pulmonary congestion and compromising
Cardiac Failure (Cardiogenic Shock (pump failure) due to excessive myocardial tissue loss or arrhythmia
Cardiac Output obstruction (pulmonary embolism, aortic dissection, pericardial tamponade)
Loss of peripheral vascular tone (Septic Shock or anaphylaxis)
![]() agonists: increase peripheral vascular resistance
agonists: increase peripheral vascular resistance
Norepinephrine, phenylephrine, metaraminol, mephenteramine and methoxamine may be used to maintain blood pressure in severe hypotension.
The objective is to ensure adequate CNS perfusion.
The use of these agents may be indicated if the hypotensive state is due to sympathetic failure, such as possibly occurring following spinal anesthesia or injury.
In shock due to other causes, reflex vasoconstriction is typically intense; adding a agonists may be harmful by further compromising organ (e.g. renal) perfusion.
ß- agonists: increase heart rate and contractility
Increasing heart rate and contractility by isoproterenol, epinephrine or norepinephrine may adversely affect cardiac performance in damaged myocardium.
These agents increase myocardial oxygen requirements and may induce arrhythmias.
Norepinephrine by increasing afterload (a receptor activation) may worsen myocardial performance
Dopamine and Dobutamine
 |
|
|
|
|
Dopamine and Dobutamine
Overview:
Dopamine (Intropin), at low concentrations, acts at D1 receptors and improve myocardial contractility (positive inotropism).
Dopamine (Intropin) produces less of an increase in heart rate compared to isoproterenol (Isuprel) and dopamine (Intropin) dilates renal arteries, promoting better kidney perfusion.
Dobutamine (Dobutrex),
through complex actions mediated by ![]() and ß receptors enhances contractility without
substantially increasing either heart rate or peripheral
resistance.
and ß receptors enhances contractility without
substantially increasing either heart rate or peripheral
resistance.
Dopamine (Intropin) and dobutamine (Dobutrex) are used for short-term inotropic support of the failing heart.
Dobutamine is less arrhythmogenic and produces less tachycardia compared to endogenous catecholamines or isoproterenol (Isuprel).
Dobutamine (Dobutrex)
Dobutamine (Dobutrex)is a racemate that binds to
and activates ![]() -1 and
-1 and
![]() -2 adrenoceptor subtypes.
-2 adrenoceptor subtypes.
The (-) enantiomer stimulates
![]() 1 and a
1 and a![]() 2 receptors, but this effect in humans appear
negated by binding of the inactive (+) enantiomer.
2 receptors, but this effect in humans appear
negated by binding of the inactive (+) enantiomer.
Therefore the positive inotropic action mediated by beta receptor activation predominates.
Dobutamine (Dobutrex) does not activate dopamine receptors and therefore does not increase renal blood flow.Because of its vasodilator properties, dobutamine's positive inotropism is accompanied by a decrease in afterload. For this reason dobutamine may be favored over dopamine for most advanced heart failure patients who have not improved with digoxin (Lanoxin, Lanoxicaps) , diuretics, and vasodilator therapy.
Dopamine (Intropin)
Dopamine (Intropin)may produce tachycardia which may increase left ventricular work.
Dopamine (Intropin)-induced vasodilation is mediated by direct stimulation of D1 and D2 post-synaptic dopamine receptors
Vasodilation of renal vasculature is noteworthy and may benefit patients with marginal GFR due to poor renal perfusion.
Drugs in Cardiogenic Shock: Nitrates, Adrenergic Agonists, Amrinone (Inocor) and Milrinone (Primacor)
In cardiogenic shock precipitated by acute myocardial infarction, salvage of reversibly damaged myocardial may be accomplished by:
supplemental oxygen
i.v. nitroglycerin (decreasing preload)
intra-aortic balloon pump (reducing afterload)
surgery to repair valve pathologies or to revascularize
Nitroglycerin
Sublingual nitroglycerin is used to relieve symptoms of angina or as a prophylactic before demanding activities that would otherwise cause angina.
Angina pectoris caused by temporary myocardial ischemia is responsive to treatment by organic nitrates.
These agents act primarily by vasodilation (especially demodulations) which reduces myocardial preload and therefore myocardial oxygen demand.
Nitrates also promote redistribution of blood flow to relatively ischemic areas.
The organic nitrates and nitrites are denitrated to produce nitric oxide (NO) which:
activates guanylyl cyclase.
Activation of cyclase results in increased concentrations of cyclic guanosine 3',5'-monophosphate (cyclic GMP) which results in vasodilation by increasing the rate of light-chain myosin dephosphorylation.
Nitric oxide synthetase produces endogenous nitrates by action on L-arginine.
Some arteriolar dilation, evidenced by flushing and dilation of meningeal arterial vessels, is responsible for headache associated with nitroglycerin use.
Cardiogenic Shock may be caused myocardial stunning due to prolonged cardiopulmonary bypass.
Dopamine (Intropin) and Dobutamine (Dobutrex) may be useful as positive inotropic agents
Dobutamine (Dobutrex) may be preferable because of a decreased likelihood of increasing heart rate and peripheral resistance (increasing afterload increases myocardial work).
Amrinone (Inocor) and milrinone (Primacor) (phosphodiesterase inhibitors) have positive inotropic effects that may be useful if other agents are ineffective.
Amrinone (Inocor) and milrinone (Primacor) are bipyridine derivatives that are relatively selective inhibitors of cGMP-inhbited, cyclic AMP phosphodiesterase (type III).
These agents cause vasodilation (decreased afterload) and increase myocardial contractility.
Milrinone (Primacor) is the agent of choice among the phosphodiesterase inhibitors for short-term parenteral support in severe heart failure patients.
Oral formulations are not used due to intolerable side-effects including increases in mortality.
Adverse Effects: Amrinone (Inocor) has been associated with a reversible thrombocytopenia.
ß adrenergic receptor agonists have had limited use in chronic management of congestive heart failure.
In congestive failure, a significant loss of ß1 receptors (50%) occurs. Loss of receptor number and desensitization limit ß adrenergic receptor agonist efficacy.
Hollenberg, S.M. and Parrillo, J.E., Shock, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, p. 215-222
Hoffman, B.B and Lefkowitz, R.J, Catecholamines, Sympathomimetic Drugs, and Adrenergic Receptor Antagonists, In, Goodman and Gillman's The Pharmacologial Basis of Therapeutics,(Hardman, J.G, Limbird, L.E, Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) The McGraw-Hill Companies, Inc.,1996, pp.222-224.
Stoelting, R.K., "Sympathomimetics", in Pharmacology and Physiology in Anesthetic Practice, Lippincott-Raven Publishers, 1999, p.259.
Clinical Manifestations and Physical Findings in Congestive Heart Failure
Dyspnea: The most common symptom of heart failure, dyspnea or respiratory distress occurs because of increased effort of breathing.
Dyspnea occurs initially upon exertion, but in advanced CHF may occur at rest.
Cardiac dypsnea is usually seen in patients with increased pulmonary venous and capillary pressure.
The combination of interstitial pulmonary edema and vessel enlargement result in reduced lung compliance and increased respiratory muscle work of breathing.
Enhanced activity of respiratory muscles further compromise available oxygen and contributes to the sensation of breathlessness.
Orthopnea, dyspnea while recumbent, is due fluid redistribution from the lower extremities into the chest with a resultant increase in pulmonary capillary hydrostatic pressure.
Paroxysmal (nocturnal) dyspnea is a sudden-onset of severe shortness of breath and coughing, awakening the patient.
Factors that produce paroxysmal dyspnea include:
depression of respiratory center during sleep (decreases arterial oxygen)
decreased ventricular function due to decreased sympathetic tone (decrease myocardial contractility and hence cardiac output) and
redistribution of fluid to the chest.
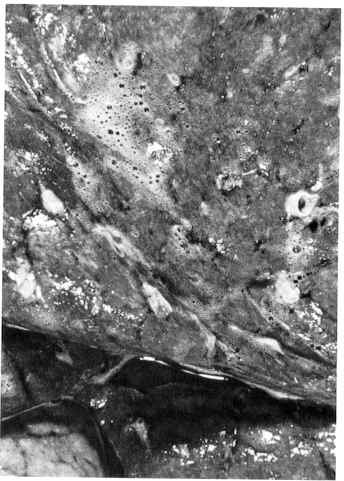 |
Initially, the edema is found in the lower lobes; however, in advanced disease all lobes may be involved.
Sectioning of the lobes reveals a sanguineous fluid consisting of a mixture of air and edema fluid.
Loop diuretics such as furosemide, bumetanide, torsemide, and ethacrynic acid are effective in reducing pulmonary edema in CHF.
By intravenous administration a pronounced naturesis may begin within minutes
Furosemide (Lasix), bumetanide (Bumex), torsemide (Demadex), and ethacrynic acid (Edecrin) are "high-ceiling" loop diuretics acting primarily at the ascending limb of the loop of Henle.
The effectiveness of these agents is related to their site of action because reabsorption of about 30 - 40% of the filtered sodium and chloride load occurs at the ascending loop.
Distal sites are not able to compensate completely for this magnitude of reduction of NaCl reabsorption.
Loop diuretics increase urinary Ca2+ in contrast to the action of thiazides.
Loop diuretics also increase renal blood flow by decreasing renal vascular resistance.
These drugs are beneficial in managing systemic and pulmonary fluid overload produced by congestive heart failure (CHF).
By i.v. administration they are particularly effective in resolving acute pulmonary edema.
Adverse Effects:
Ototoxicity
Furosemide and ethacrynic acid block renal excretion of uric acid by competition with renal secretory and biliary secretory systems.Therefore these agents can precipitate gout.
Potassium depletion.
Figure and description above adapted from "Robbins: The Pathological Basis of Disease" Fifth Edition, p. 96
|
|
|
![]()
Cardiac asthma, related to paroxysmal dyspnea, is characterized by wheezing due to bronchospasm.
Acute pulmonary edema, however, involves a significant elevation of pulmonary capillary pressure leading to alveolar edema, extreme shortness of breath and rales.
Expectoration of blood-tinged fluid may occur.
Acute pulmonary edema may be fatal.
Fatigue, weakness and reduced exercise capacity are common in congestive heart failure patients.
Exercise capacity is reduced because increased cardiac output required to support increased levels of physical activity is unavailable or inadequate.
Pulmonary Rales
Peripheral (cardiac) edema is commonly seen symmetrically in the legs, particular in the pretibial region and ankles.
|
|
|
Ascites and pleural effusion. Pleural effusion results from increased pulmonary capillary hydrostatic pressure and the attendant movement of fluid into the pleural cavity.
Congestive Hepatomegaly
Jaundice
Cardiac Cachexia. Serious weight loss and cachexia may occur in chronic, severe congestive heart failure due to:
increased circulating tumor necrosis factor
hepatomegaly, and abdominal fullness
increased metabolic rate need to support the increased effort of breathing
impairment of intestinal absorption due to intestinal venous congestion
anorexia, nausea, vomiting due to digitalis intoxication, congestive
protein-losing enteropathy (rare)
Aspects of Digitalis (cardiac glycosides)
|
|
|
|
Cardiac glycosides are inhibitors of sodium and potassium transmembrane transport by binding to the alpha subunit of Na+ -K+ -ATPase.
The structure of digoxin is shown at the right and the lactone, steroid nucleus, and sugar residue component moieties illustrated.
Removal of the glycoside moiety only minimally affects Na+ -K+ -ATPase binding but changes pharmacokinetic behavior. With the glycoside component removed, the resultant molecule is the "genin" or "aglycone".
Digitoxin differs from digoxin only by the lack of a hydroxyl group at C12. This difference changes the hydrophilicity of the compound and affects its pharmacokinetics.
top figure: from: "Goodman and Gilman's The Pharmacological Basis of Therapeutics, Ninth Edition, p. 810.
Positive inotropic responses to cardiac glycosides results from increasing calcium concentrations in the vicinity of myofilaments during excitation.
Increased calcium is secondary to an increase in intracellular sodium which occurs because of Na+ -K+ -ATPase inhibition. Na+ -K+ -ATPase inhibition is caused by digitalis.
"Applied Therapeutics: The Clinical Use of Drugs", Sixth edition, edited by Lloyd Lee-Young and Mary Ann Koda-Kimble, p 15-5, Applied Therapeutics, Inc., 1995, Seattle, WA.
Prolongation of the effective refractory period by enhancement of vagal tone.
High concentration: increased diastolic depolarization and decreased resting membrane potential lead to enhanced automaticity and ectopy.
![]()
Quinidine and Digitalis Combination Treatment: Context
Quinidine administration results in vagal inhibition (anti-muscarinic).
The antimuscarinic effect of quinidine facilitates transmission of atrial impulses to the ventricles
In atrial fibrillation such action can increase ventricular rate.
To protect against this effect digitalis (digoxin/digitoxin) may be administered because digitalis inhibits transmission through the AV node.
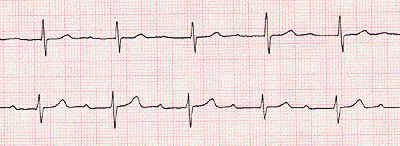
Digitalis glycosides & Atrial fibrillation
Atrial fibrillation may result in a high ventricular rate.
Drugs which reduce ventricular rate by reducing AV nodal conduction include:
Digitalis glycosides
calcium channel blockers
ECG rhythm strip illustrating atrial fibrillation. Note the absence of "P" waves and the irregularly irregular spaced QRS complexes.
.
Other Useful Drugs
Calcium channel blockers
Blocks cardiac calcium channels in slow response tissues, such as the sinus and AV nodes.
Useful in treating AV reentrant tachyarrhythmias and in management of high ventricular rates secondary to atrial flutter or fibrillation.
Major adverse effect (i.v. administration) is hypotension. Heart block or sinus bradycardia can also occur.
ß-adrenergic receptor blockers
Antiarrhythmic effects are due mainly to beta-adrenergic receptor blockade. Normally, sympathetic drive results in increased in Ca2+ ,K+ ,and Cl- currents.
Increased sympathetic tone also increases phase 4 depolarization (heart rate goes up), and increases DAD (delayed afterdepolarizations) and EAD (early afterdepolarization) mediated arrhythmias. These effects are blocked by beta-adrenergic receptor blockers.
![]() -adrenergic receptor
blockers increase AV conduction time and increase
AV nodal refractoriness, thereby helping to terminate
nodal reentrant arrhythmias.
-adrenergic receptor
blockers increase AV conduction time and increase
AV nodal refractoriness, thereby helping to terminate
nodal reentrant arrhythmias.
![]() -adrenergic receptor
blockade can also help reduce ventricular
following rates in atrial flutter and
fibrillation, again by acting at the AV node.
-adrenergic receptor
blockade can also help reduce ventricular
following rates in atrial flutter and
fibrillation, again by acting at the AV node.
Adverse effects of beta blocker therapy can lead to fatigue, bronchospasm, depression, impotence, and attenuation of hypoglycemic symptoms in diabetic patients and worsening of severe congestive heart failure.
Quinidine assists in restoring and maintaining normal sinus rhythm
Although classified as a sodium channel blocker, quinidine also blocks K+ channels. Most antiarrhythmic agents have such multiple actions.
Sodium channel blockade results in an increased threshold and decreased automaticity.
Potassium channel blockade results in AP prolongation.
Quindine is used to maintain normal sinus rhythm in patients who have experienced atrial flutter or fibrillation. Also, it is used to prevent ventricular tachycardia or fibrillation.
Quinidine administration results in vagal inhibition (anti-muscarinic) and alpha-adrenergic receptor blockade.
Adverse effects include cinchonism (headaches and tinnitus), diarrhea.
Quinidine is also associated with torsades de pointes, a ventricular arrhythmias associated with marked QT prolongation. This potentially serious arrhythmia occurs in 2% - 8% if patients, even if they have a therapeutic or subtherapeutic quinidine blood level.
Central Nervous System effects:
Psychiatric: delirium, fatigue, abnormal dreams
Visual: disturbed color vision
Gastrointestinal: anorexia, nausea, vomiting, abdominal pain
Cardiac: proarrhythmic effects
Ectopic beats of AV junctional or ventricular origin.
First-degree AV block
Sinus bradycardia
Ventricular arrhythmias
Antidigoxin immunotherapy is an effective antidote for digitalis intoxication and is based on digoxin-specific Fab fragments.
Potassium administration and used of phenytoin or lidocaine be useful in managing serious ventricular arrhythmias.
Amrinone (Inocor) /Milrinone (Primacor)
Amrinone (Inocor) and milrinone (Primacor) are bipyridine derivatives that are relatively selective inhibitors of cGMP-inhbited, cyclic AMP phosphodiesterase (type III).
These agents cause vasodilation (decreased afterload) and increase myocardial contractility.
Milrinone (Primacor) is the agent of choice among the phosphodiesterase inhibitors for short-term parenteral support in severe heart failure patients.
Oral formulations are not used due to intolerable side-effects including increases in mortality.
Adverse Effects: Amrinone has been associated with a reversible thrombocytopenia.
Angiotensin II, a potent vasoconstrictor, is produced by the action of angiotensin converting enzyme (ACE) on the substrate angiotensin I.
Angiotensin II activity produces:
(a) a rapid pressor response
(b) a slow pressor response
(c) vascular and cardiac hypertrophy and remodeling.
Benefits of ACE inhibitors in treating congestive heart failure and antihypertension are due to the reduction in the amount of angiotensin II produced.
Reduction in angiotensin II levels results in venous and arterial vasodilation which decreases both preload and afterload.
Cardiac output improvement reduces sympathetic tone which may further decrease peripheral resistance.
Use of ACE inhibitors improves survival (40%) in patients with overt heart failure (CONSENSUS,1987 study).
ACE inhibitors are efficacious in management of congestive heart failure and hypertension and have a favorable side effect profile.
ACE inhibitor are advantageous in management of diabetic patients by reducing the development of diabetic neuropathy and glomerulosclerosis.
ACE inhibitor are probably the antihypertensive drug of choice in treatment of hypertensive patient who have hypertrophic left ventricles.
Hypertensive patients who have ischemic heart disease with impaired left ventricular function also benefit from ACE inhibitor treatment.
ACE inhibitors reduce the normal aldosterone response to sodium loss (normally aldosterone opposes diuretic-induced sodium loss).
Therefore, the use of ACE inhibitors enhance the efficacy of diuretic treatment, allowing the use of lower diuretic dosages and improving control of hypertension.
If diuretics are administered at higher dosages in combination with ACE inhibitors significant and undesirable hypotensive reactions can occur with attendant excessive sodium loss.
Reduction in aldosterone production by ACE inhibitors also affects potassium levels. The tendency is for potassium retention, which may be serious in patients with renal disease or if the patient is also taking potassium sparing diuretics, nonsteroidal anti-inflammatory agents or potassium supplements.
Adverse Effects:
Angioedema, although rare, may be potentially fat
ACE inhibitors should not be used during pregnancy.
Dry cough.
In renovascular hypertension, glomerular filtration pressures are maintained by vasoconstriction of the post-glomerular arterioles, an effect mediated by angiotensin II. Used of ACE inhibitors in patients with renovascular hypertension due to bilateral renal artery stenosis can therefore precipitate a significant reduction in GFR and acute renal failure.
Initial dose of an ACE inhibitor may precipitate an excessive hypotensive response.
High-ceiling loop diuretics and fluid load reduction in congestive heart failure.
Fluid Load Reduction in Congestive Heart Failure
Loop Diuretcs: Inhibitors of Na+-K+-2Cl- Synport
|
 |
|
 |
| Top Figure: Guyton's Textbook of Physiology, Ninth Edition, p. 318. | Bottom Figure: Goodman and Gillman's "The Pharmacological Basis of Therapeutics", Ninth Edition, p. 699 |
![]()
Drugs Used in Management of Congestive Heart Failure
Digitalis
Digoxin (Lanoxin, Lanoxicaps,) Digitoxin
Digitalis glycosides are composed of a steroid nucleus to which an unsaturated lactone ring is attached at C-17. These two components, the aglycone or genin moieties, are responsible for the inotropic activity of glycosides.
Digoxin has a half-life of about 1.6 days. By contrast digitoxin's half-life is about 5 days. Digitoxin is rarely used and may no longer be readily available in the United States.
Digoxin is mainly excreted in the urine (85%). By contrast digitoxin is mainly metabolized in the liver.
Ouabain is very rapidly acting (5 to 10 min onset) after i.v. injection.
The clinical efficacy of digitalis glycosides is based on improving cardiac contractility (positive inotropism) and on decreasing transmission through the A-V node.
The most important cardiac effect is the shift of the force-velocity relationship upward.
Bipyridines
Amrinone (Inocor) and milrinone (Primacor) are bipyridine derivatives that are relatively selective inhibitors of cGMP-inhbited, cyclic AMP phosphodiesterase (type III).
These agents cause vasodilation (decreased afterload) and increase myocardial contractility.
Milrinone (Primacor) is the agent of choice among the phosphodiesterase inhibitors for short-term parenteral support in severe heart failure patients.
Oral formulations are not used due to intolerable side-effects including increases in mortality.
Amrinone has been associated with a reversible thrombocytopenia.
Adrenergic agonists: Dopamine (Intropin), Dobutamine (Dobutrex); Dopamine (Intropin) and dobutamine (Dobutrex) are used for short-term inotropic support of the failing heart.
Dobutamine (Dobutrex) is less arrhythmogenic and produces less tachycardia compared to endogenous catecholamines or isoproterenol (Isuprel).
Dobutamine (Dobutrex)
Dobutamine (Dobutrex) is a
racemate that binds to and activates ![]() -1 and
-1 and
![]() -2 adrenoceptor subtypes.
-2 adrenoceptor subtypes.
The (-) enantiomer
stimulates ![]() 1 and
1 and ![]() 2 receptors,
but this effect in humans appear negated
by binding of the inactive (+) enantiomer.
2 receptors,
but this effect in humans appear negated
by binding of the inactive (+) enantiomer.
Therefore the positive inotropic action mediated by beta receptor activation predominates.
Dobutamine (Dobutrex) does not activate dopamine receptors and therefore does not increase renal blood flow.
Because of its vasodilator properties, dobutamine's positive inotropism is accompanied by a decrease in afterload. For this reason dobutamine may be favored over dopamine for most advanced heart failure patients who have not improved with digoxin, diuretics, and vasodilator therapy.
Dopamine (Intropin)
Dopamine (Intropin)may produce tachycardia which may increase left ventricular work.
Dopamine (Intropin)-induced vasodilation is mediated by direct stimulation of D1 and D2 post-synaptic dopamine receptors.
Vasodilation of renal vasculature is noteworthy and may benefit patients with marginal GFR due to poor renal perfusion.
Vasodilators (Hydralazine (Apresoline), Minoxidil (Loniten))
Vasodilators may be used in the management of congestive heart failure as a means of reducing afterload.
Hydralazine (Apresoline) and minoxidil (Loniten) are the prominent members of the class, although minoxidil is preferred.
Both drugs can induce reflex-mediated cardiac stimulation and water retention although in patients with advanced failure significant sympathetic tone may already be present. In that situation intervention that improve cardiac output and tissue perfusion may actually reduce overall sympathetic activity.
Vasodilator therapy is typically not used initially. ACE inhibitors, diuretics and digoxin would be likely tried first. More aggressive diuretic treatment and/or addition of vasodilators could follow.
Adverse effects include those induced by vasodilation such as hypotension, palpitation, tachycardia, angina, fluid retention and headache.
A drug-induced lupus syndrome is associated with hydralazine.
A drug-induced hypertrichosis is associate with minoxidil
Loop Diuretics: Furosemide (Lasix), Bumetanide (Bumex, Ethacrynic acid (Edecrin)
Furosemide (Lasix), bumetanide (Bumex), torsemide (Demadex), and ethacrynic acid (Edecrin) are "high-ceiling" loop diuretics acting primarily at the ascending limb of the loop of Henle.
The effectiveness of these agents is related to their site of action because reabsorption of about 30 - 40% of the filtered sodium and chloride load occurs at the ascending loop.
Distal sites are not able to compensate completely for this magnitude of reduction of NaCl reabsorption.
Loop diuretics increase urinary Ca2+ in contrast to the action of thiazides.
Loop diuretics also increase renal blood flow by decreasing renal vascular resistance.
These drugs are beneficial in managing systemic and pulmonary fluid overload produced by congestive heart failure (CHF).
By i.v. administration they are particularly effective in resolving acute pulmonary edema.
Adverse Effects:
Ototoxicity
Furosemide (Lasix) and ethacrynic acid (Edecrin) block renal excretion of uric acid by competition with renal secretory and biliary secretory systems.Therefore these agents can precipitate gout.
Potassium depletion.
ACE Inibitors: Three Major Effects of Angiotensin II and Underlying Mechanisms
 |
Benazepril (Lotensin)
Captopril (Capoten): Prototype drug
Angiotensin II, a potent vasoconstrictor, is produced by the action of angiotensin converting enzyme (ACE) on the substrate angiotensin I.
Angiotensin II activity produces:
(a) a rapid pressor response
(b) a slow pressor response
(c) vascular and cardiac hypertrophy and remodeling.
ACE inhibitors are efficacious in management of congestive heart failure and hypertension and have a favorable side effect profile.
Benefits of ACE inhibitors in treating congestive heart failure and antihypertension are due to the reduction in the amount of angiotensin II produced. Reduction in angiotensin II levels results in venous and arterial vasodilation which decreases both preload and afterload. Cardiac output improvement reduces sympathetic tone which may further decrease peripheral resistance.
Use of ACE inhibitors improves survival (40%) in patients with overt heart failure (CONSENSUS,1987 study).
ACE inhibitor are advantageous in management of diabetic patients by reducing the development of diabetic neuropathy and glomerulosclerosis.
ACE inhibitor are probably the antihypertensive drug of choice in treatment of hypertensive patient who have hypertrophic left ventricles. Hypertensive patients who have ischemic heart disease with impaired left ventricular function also benefit from ACE inhibitor treatment.
ACE inhibitors reduce the normal aldosterone response to sodium loss (normally aldosterone opposes diuretic-induced sodium loss).
Therefore, the use of ACE inhibitors enhance the efficacy of diuretic treatment, allowing the use of lower diuretic dosages and improving control of hypertension.
If diuretics are administered at higher dosages in combination with ACE inhibitors significant and undesirable hypotensive reactions can occur with attendant excessive sodium loss.
Reduction in aldosterone production by ACE inhibitors also affects potassium levels.
The tendency is for potassium retention, which may be serious in patients with renal disease or if the patient is also taking potassium sparing diuretics, nonsteroidal anti-inflammatory agents or potassium supplements.
Adverse Effects
Angioedema, although rare, may be potentially fatal.
ACE inhibitors should not be used during pregnancy.
Dry cough.
In renovascular hypertension, glomerular filtration pressures are maintained by vasoconstriction of the post-glomerular arterioles, an effect mediated by angiotensin II.
Use of ACE inhibitors in patients with renovascular hypertension due to bilateral renal artery stenosis can therefore precipitate a significant reduction in GFR and acute renal failure.
Initial dose of an ACE inhibitor may precipitate an excessive hypotensive response.
Enalapril (Vasotec)
Fosinopril (Monopril)
Lisinopril (Prinvivil)
Moexipril (Univasc)
Quinapril (Accupril)
Ramipril (Altace)