|
press  above to
begin the lecture above to
begin the lecture
return to Pharmacology Table
of Contents
Table
of Contents
-
ß2 selective adrenergic
agonists
-
a-Selective
Adrenergic Agonists
-
a2
Selective
Adrenergic Agonists
-
Introduction
-
Clonidine
(Catapres)
-
Guanfacine
(Tenex)
-
Guanabenz
(Wytensin)
-
a-methyl DOPA
(Aldomet)
-
Miscellaneous
Amphetamine
-
Clinical Use of Sympathomimetic
Agents
|
-
Amphetamines
-
Adrenergic
Neuronal Blocking Drugs
-
Classification of
adrenoceptors (
a1, a2,ß1,
ß2
and D1), molecular consequences of their
activation, and their important locations.
-
Catecholamine
Metabolic Transformations
-
Pulmonary
Uptake
-
Adrenergic
and Cholinergic Effects on End Organs
-
Clinical
Uses: Sympathomimetic Drugs: a/b Adrenergic Agonists
-
Therapeutic
Uses of Indirect-Acting Adrenergic Agonists
-
Adverse
Effects: b Adrenergic Antagonists
-
a-Adrenergic
Antagonists
-
Introduction
-
a1-adrenergic
receptor antagonists
-
a2-adrenergic receptor antagonists
-
Phenoxybenzamine
(Dibenzyline)
-
Phentolamine(Regitine)
and tolazoline (Priscoline)
-
Prazosin
(Minipress) and Terazosin (Hytrin)
-
Others
-
b Adrenergic
Antagonists
-
Introduction
-
ß receptor blockers: Effects
on the heart
-
ß receptor blockers:
Antihypertensive
Effects
-
Pulmonary
Effects
-
Metabolic
Actions
-
Nonselective-ß adrenergic
receptor antagonists
-
propranolol
-
nadolol
-
timolol
-
labetalol
-
Cardioselective ß1 adrenergic
receptor antagonists
-
metoprolol
-
esmolol
-
atenolol
-
Adverse Effects of ß
adrenergic
receptor antagonists
-
Therapeutic
Uses
|
Norepinephrine
Blood Pressure
-
Potent vasopressor
-
Systolic and
diastolic pressure increase
-
Norepinephrine (Levophed) increases blood
pressure by:
-
vasoconstriction
a1
receptor
effects
-
Elevation
of systolic pressure following
norepinephrine is likely to
activate the baroreceptor system resulting in a reflex-mediated
decrease in heart rate.
Blood Pressure
Blood
Pressure Effects
|
Epinephrine
|
Norepinephrine
|
|
Systolic
|
  
|
  
|
|
Mean Pressure
|

|
 
|
|
Diastolic
|
variable
|
 
|
|
Mean Pulmonary
|
 
|
 
|
0.1-0.4
ug/kg/min IV infusion
Adaptation of Table 10-2 from: Hoffman,
B.B and Lefkowitz, R.J, Catecholamines, Sympathomimetic
Drugs, and Adrenergic Receptor Antagonists, In, Goodman
and Gillman's The Pharmacologial Basis of Therapeutics,(Hardman, J.G,
Limbird, L.E, Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) The McGraw-Hill
Companies, Inc.,1996, pp.199-242
Arterioles (Adrenergic Effects in RED; Cholinergic Effects
in
BLUE)
|
Coronary
|
alpha1,2; beta 2
|
constriction;dilatation
|
constriction
|
|
Skin/Mucosa
|
alpha1,2
|
constriction
|
dilatation
|
|
Skeletal Muscle
|
alpha; beta2
|
constriction,dilatation
|
dilatation
|
|
Cerebral
|
alpha1
|
slight
constriction
|
dilatation
|
|
Pulmonary
|
alpha1
, beta2
|
constriction;
dilatation
|
dilatation
|
|
Abdominal viscera
|
alpha1, beta2
|
constriction;
dilatation
|
-------
|
|
Salivary glands
|
alpha1,2
|
constriction
|
dilatation
|
|
Renal
|
alpha1,2;beta1,2
|
constriction;dilatation
|
---------
|
Based on Table 6-1: Lefkowitz, R.J, Hoffman, B.B and Taylor, P. Neurotransmission: The
Autonomic and Somatic Motor Nervous Systems, In, Goodman
and Gillman's The Pharmacologial Basis of Therapeutics,(
Hardman, J.G, Limbird, L.E, Molinoff, P.B., Ruddon, R.W,
and Gilman, A.G.,eds) TheMcGraw-Hill Companies,
Inc.,1996, pp.110-111.
Vascular
Effects
-
Norepinephrine significantly
increases total peripheral resistance,
often inducing reflex cardiac slowing.
-
Norepinephrine
(Levophed)
causes vasoconstriction in most vascular
beds.
-
Blood flow is reduced to the
kidney, liver and skeletal muscle.
-
Glomerular filtration rates
are usually maintained.
-
Norepinephrine may increase
coronary blood flow (secondary to
increased blood pressure and reflex
activity)
-
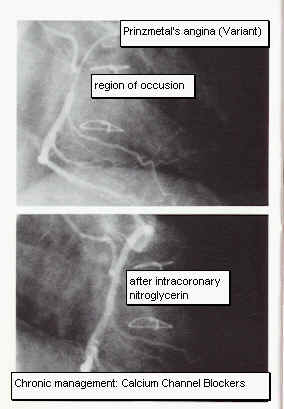
Norepinephrine
(Levophed) may
induce variant (Prinzmetal's) angina.
-
Pressor effects of
norepinephrine (Levophed) are blocked by
alpha-receptor blockers.
-
ECG changes following
norepinephrine (Levophed) are variable,
depending on the extent of reflex vagal
effects.
Peripheral Circulation
Peripheral
Circulation
|
Epinephrine
|
Norepinephrine
|
|
Total Peripheral
Resistance
|

|
 
|
|
Cerebral Blood Flow
|

|
no effect
or decrease
|
|
Muscle Blood Flow
|
  
|
no effect
or decrease
|
|
Cutaneous Blood Flow
|
 
|
 
|
|
Renal Blood Flow
|

|

|
|
Splanchnic Blood Flow
|
  
|
no effect or increase
|
 increase,
increase,  decrease decrease
0.1-0.4
ug/kg/min IV infusion
Adaptation of Table 10-2 from:
Hoffman, B.B and Lefkowitz, R.J, Catecholamines,
Sympathomimetic Drugs, and Adrenergic Receptor
Antagonists, In, Goodman and Gillman's The Pharmacologial
Basis of Therapeutics, Hardman, J.G, Limbird, L.E, Molinoff, P.B.,
Ruddon, R.W, and Gilman, A.G.,eds) The
McGraw-Hill Companies, Inc.,1996, pp.199-242
Therapeutic use:
Norepinephrine
Hoffman, B.B and Lefkowitz, R.J,
Catecholamines, Sympathomimetic Drugs, and Adrenergic Receptor
Antagonists, In, Goodman and Gillman's The Pharmacologial Basis of
Therapeutics, (Hardman, J.G, Limbird, L.E, Molinoff, P.B., Ruddon, R.W,
and Gilman, A.G.,eds) TheMcGraw-Hill Companies, Inc.,1996, pp.204-213.

return to Table of Contents
Dopamine
Cardiovascular
Effects (Dopamine)
-
Vasodilator:
-
At low doses,
dopamine (Intropin) interactions
with D1 receptor
subtype results in renal,
mesenteric and coronary vasodilation.
-
Low doses result
in enhancing glomerular
filtration rates (GFR), renal
blood flow, and sodium excretion.
-
Positive
inotropism:
-
At higher doses,
dopamine increase myocardial
contractility through activation
of ß1 adrenergic
receptors
-
Dopamine
(Intropin) also promotes release
of myocardial norepinephrine.
-
Dopamine
(Intropin) at these higher
dosages causes an increase in
systolic blood and pulse pressure
with little effect on diastolic pressures.
-
Vasopressor:
Therapeutic use (Dopamine)
Unique
among catecholamines in that Dopamine can
simultaneously increase
|
myocardial
contractility
|
glomerular
filtration rate
|
sodium
excretion
|
urine
output
|
renal
blood flow
|
-
Increased
sodium excretion following dopamine may
be due to inhibition of aldosterone
secretion.
-
Dopamine
may inhibit renal tubular solute
reabsorption(suggesting that natriuresis
& diuresis may occur by different
mechanisms.)
-
Fenoldopam
and dopexamine: newer drugs
-
Dopamine
(Intropin) at higher doses increases
myocardial contractility by ß1
- adrenergic receptor activation.
-
Ventilation effects: --
dopamine IV infusion interferes with
ventilatory responses to arterial
hypoxemia
Dopamine
(Intropin) acts as inhibitory neurotransmitter at carotid
bodies)

return to Table of Contents
Dopexamine
-
Dopexamine--synthetic
catecholamine
-
Activation of dopaminergic and
beta2 receptors
-
Slight positive inotropic effect
(beta2-adrenergic agonists activity; potentiation
those endogenous norepinephrine secondary to
reuptake blockade)
-
Dopexamine
enhances creatinine clearance

return to Table of Contents
Isoproterenol
(Isuprel)
-
Activates ß adrenergic
receptors (both ß1 - and ß2
-receptor subtypes)
-
Has limited action at a
adrenergic receptors
-
i.v. influsion of isoproterenol
results in a slight decrease in mean blood
pressure with a marked drop in diastolic
pressure.
-
ß2 - adrenergic
receptor-mediated reduction in peripheral
resistance (reflected in the diastolic pressure
effects) is primarily due to vasodilation of
skeletal muscle vasculature. Renal and mesenteric
vascular beds are also dilated.
-
Activation of cardiac ß1
- adrenergic receptors: increased contractility
and heart rate.
-
Activation of ß2 -
adrenergic receptors: Bronchial and GI smooth
muscle relaxation.
-
Isoproterenol and ß2
-selective adrenergic agonists inhibit
antigen-mediated histamine release.
Isoproterenol: Limited therapeutic uses:


return to Table of Contents
Dobutamine
(Dobutrex)
-
Structurally
similar to dopamine (Intropin).
Pharmacological effects exerted
through interaction with a and
ß adrenergic receptor interactions
-
Pharmacological effects are due to
complex interactions of (-) and (+) enantiometic
forms present in the clinically used racemate
with a and ß
adrenergic receptors.
-
Dobutamine (Dobutrex) is a positive
inotropic agent usually causing limited increase
in heart rate.
Dobutamine (Dobutrex): Adverse Effects
-
Significant blood pressure
and heart rate increases may occur.
-
Ventricular ectopy
-
Increased ventricular
following rate in patient with atrial
fibrillation.
-
Increased myocardial
oxygen demand that may worsen
post-infarct myocardial damage
|
Dobutamine
(Dobutrex): Therapeutic Use
-
Short-term management of pump
failure following surgery, during acute
congestive heart failure, or
post-myocardial infarction.
-
Uncertain long-term
efficacy.
|
Hoffman, B.B and Lefkowitz, R.J, Catecholamines, Sympathomimetic Drugs, and Adrenergic
Receptor Antagonists, In, Goodman and Gillman's The
Pharmacologial Basis of Therapeutics,(Hardman, J.G, Limbird, L.E,
Molinoff, P.B., Ruddon, R.W, and Gilman, A.G.,eds) TheMcGraw-Hill Companies, Inc.,1996, pp.199-242
return to Table of
Contents
press the purple
arrow below (right) to go to the next page
|